Working with human breast and lung cells, Johns Hopkins Medicine scientists say they have charted a molecular pathway that can lure cells down a hazardous path of duplicating their genome too many times, a hallmark of cancer cells.
The findings reveal what goes wrong when a group of molecules and kinases are triggered to regulate the cell cycle, resulting in replication of chromosomes in cells that exit the cell cycle. The findings, the team suggest, could be used to develop therapies that interrupt these abnormal events in the cell cycle, and have the potential to stop the growth of cancers.
“An enduring question among scientists in the cancer field is: How do cancer cell genomes get so bad?” says Sergi Regot, PhD, associate professor of molecular biology and genetics at the Johns Hopkins University School of Medicine. “Our study challenges the fundamental knowledge of the cell cycle and makes us reevaluate our ideas about how the cycle is regulated.”
Regot and colleagues reported on their findings in Science, in a paper titled “CDK4/6 activity is required during G2 arrest to prevent stress-induced endoreplication.”
To replicate, cells follow an orderly routine that begins with making a copy of their entire genome. This is then followed by separation of the genome copies, and finally, the replicated DNA is divided evenly into two “daughter” cells. Human cells have 23 pairs of each chromosome—half from the mother and half from the father—including the X and Y sex chromosomes. This makes 46 total, but cancer cells are known to go through an intermediate state that has double that number—92 chromosomes. But how this happens was a mystery.
As the authors explained, abnormal DNA content is one of the most common characteristics of cancer cells, with recent evidence suggesting that 35 to 40 percent of tumors go through a whole-genome doubling (WGD) event as they evolve. “WGD is associated with genome instability, metastasis, and worse overall prognosis,” the team wrote, “However, the molecular mechanisms that drive WGD are poorly understood.”
Regot noted that cells that are stressed after copying the genome can enter a dormant, or senescent stage, and mistakenly run the risk of copying their genome again. And while generally and eventually, these dormant cells are swept away by the immune system after they are recognized as faulty, there are times, especially as humans age, when the immune system can’t clear the cells.
Left alone the abnormal cells can replicate their genome again, shuffle the chromosomes at the next division, and a growing cancer begins. A model known as endoreplication, the team explained in their paper, is when the cell undergoes two rounds of DNA replication without cell division. Endoreplication, they noted, contradicts the idea of irreversible commitment to cell division of cells entering the cell cycle. “We rationalized that although DNA replication and cell division are coupled under normal circumstances, there must be away to uncouple these events during times of cellular stress and break the commitment to cell division even after DNA replication has occurred.”
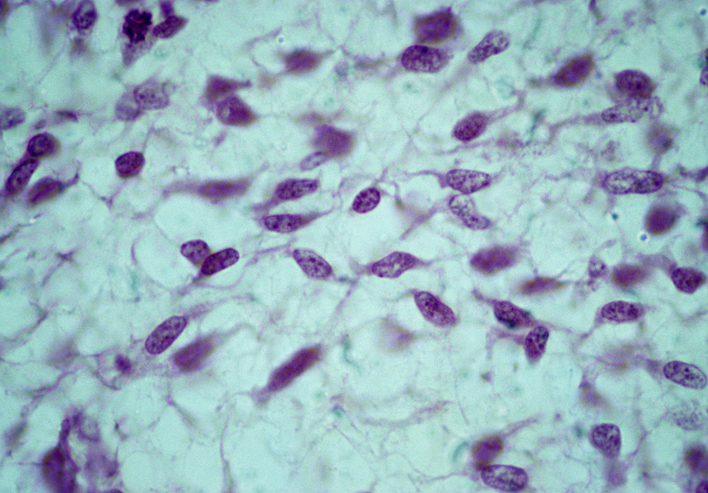
In an effort to pin down details of the molecular pathway that goes awry in the cell cycle, Regot and graduate research assistant Connor McKenney, who led the Johns Hopkins team, focused on human cells that line breast ducts and lung tissue. These cells generally divide at a more rapid pace than other cells in the body, increasing the opportunities to visualize the cell cycle. “
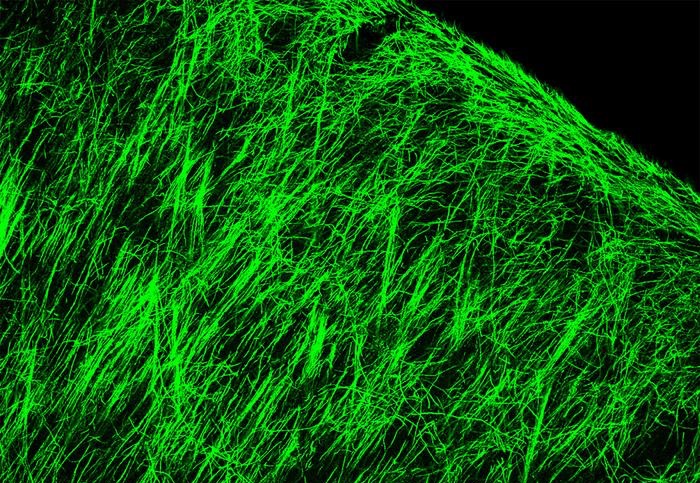
Regot’s lab specializes in imaging individual cells, making it especially suited to spot the very small percentage of cells that don’t enter the dormant stage and continue replicating their genome. For their newly reported study the team scrutinized thousands of images of single cells as they went through cell division. The researchers developed glowing biosensors to tag cyclin dependent kinases (CDKs), cellular enzymes that are known for their role in regulating the cell cycle. “Cell cycle events are coordinated by cyclin-dependent kinases (CDKs) to ensure robust cell division,” they wrote. “CDK4/6 and CDK2 regulate the growth 1 (G1) to synthesis (S) phase transition of the cell cycle …”.
Through their studies the team saw that a variety of CDKs activated at different times during the cell cycle. After the cells were exposed to an environmental stressor, such as a drug that disrupts protein production, UV radiation or osmotic stress (a sudden change in water pressure around cells), the researchers saw that CDK 4 and CDK 6 activity decreased.
Then, five to six hours later, when the cells started preparations to divide, CDK 2 was also inhibited. At that point, a protein complex called the anaphase promoting complex (APC) was activated during the phase just before mitosios—the step during which the cell pulls apart and divides. “In the stressed environment in the study, APC activation occurred before mitosis, when it’s usually been known to activate only during mitosis,” said Regot.
About 90 percent of breast and lung cells leave the cell cycle and enter a quiet state when exposed to any environmental stressors. In the scientists’ experimental cells not all of the cells went quiet. The research team discovered that five to ten percent of the breast and lung cells returned to the cell cycle, dividing their chromosomes again. “Upon relief of stress, a significant fraction of cells underwent a second round of DNA replication that led to whole-genome doubling,” they wrote.
Through another series of experiments the team linked an increase in activity of stress activated protein kinases (SAPKs) to the percentage of cells that skirt the quiet stage and continue to double their genome. “Mechanistically, G2 cell cycle exit occurs by premature activation of the anaphase-promoting complex or cyclosome (APC/C) in G2,” they wrote. “Notably, we found that premature APC/C reactivation occurs by persistent simultaneous inhibition of cyclin-dependent kinase 1 (CDK1) and CDK4/6 in G2 by SAPKs.”
The mechanisms, they noted, occurred independently of the p53 protein. “We found that SAPKs promote APC/C reactivation in G2 independently of p53.” This premature APC/C reactivation led to endoreplication of the genome in the small number of cells. “Stress-induced APC/C reactivation was driven by CDK4/6 inhibition during G2 arrest, challenging the classic definition of the restriction point and highlighting an important role of CDK4/6 beyond the G0 to G1 transition,” they noted.
Regot says there are ongoing clinical trials testing DNA-damaging agents with drugs that block CDK. “It’s possible that the combination of drugs may spur some cancer cells to duplicate their genome twice and generate the heterogeneity that ultimately confers drug resistance,” says Regot. “There may be drugs that can block APC from activating before mitosis to prevent cancer cells from replicating their genome twice and prevent tumor stage progression.” The authors further pointed out that SAPK signaling plays a central role in a variety of stress conditions that are related to aging, including proteotoxic stress, oxidative stress, and inflammation.
In the context of their study findings, they concluded, “Because SAPK-induced endoreplication is independent of p53 and most cancers with WGD lose p53 function prior to genome duplication, we propose that SAPK-mediated WGD might contribute to genetic instability and tumorigenesis in aging tissues.”
In an associated perspective in Science, Bart Westendorp, PhD, at Utrecht University, and Regenerative Medicine Center Utrecht, commented, “Given that CDK4/6 inhibition is now standard-of-care therapy for estrogen receptor–positive breast cancer, it is important to study whether these inhibitors may promote unwanted whole genome doubling events and genomic instability in patients … To answer such questions, innovative approaches will be needed for in vivo tracking of the long-term fates and clonal outgrowth of tetraploid cells arising from the G2 phases in which CDK4/6 activity is disrupted.”