A team of investigators led by scientists at Penn State University has found an interesting new way to create proteins that can slip through HIV’s protective coating—providing a potential path toward understanding the key components needed for developing a vaccine for the deadly virus. The researchers incorporated a computational modeling approach to create proteins that mimicked different surface features of HIV.
Findings from the new study—published today in Nature Communications through an article titled “Rationally designed carbohydrate-occluded epitopes elicit HIV-1 Env-specific antibodies”—showed that after being immunized with the newly designed proteins, rabbits developed antibodies that were able to bind with the virus. These results provide a novel way to design proteins for vaccines.
“We were able to show that by using our designed proteins, the blood was able to spontaneously generate antibodies that can inhibit the infection of HIV in cellular models,” explains lead study investigator Cheng Zhu, PhD, a postdoctoral fellow at Penn State College of Medicine. “When we incubated the HIV virus, its infectivity was dramatically reduced by the rabbits’ blood.”
Zhu adds that “the proteins—or immunogens—we developed aren’t a finished product, but we were able to show evidence that it’s possible to do. Moreover, it’s also very exciting that we were able to create a new method to tailor make proteins, which could open the door for developing vaccines for other infections, as well.”
While millions of people are living with HIV across the globe, creating a vaccine for the virus has alluded researchers. Vaccines work by teaching the immune system where on a virus an antibody can attach before neutralizing it. To create a vaccine, researchers first must identify this spot.
“Even if we develop an antibody for a particular strain of the virus, that antibody may not even notice the next strain of the virus,” notes senior study investigator Nikolay Dokholyan, PhD, professor and vice chair for research in the department of pharmacology at Penn State. “In order to develop broadly neutralizing antibodies—antibodies that neutralize multiple strains of a virus—we need to find something that remains constant on the virus for those antibodies to latch onto.”
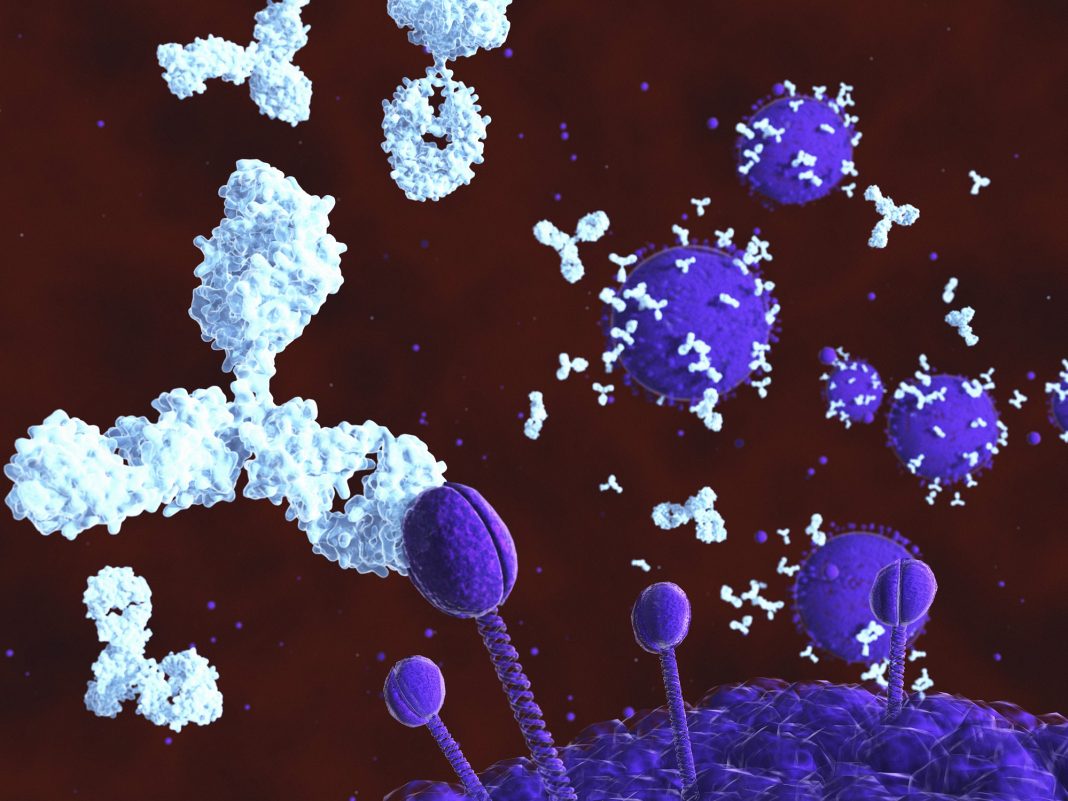
HIV uses a coating of carbohydrates to protect a protein on its surface called Env. While this protein could be a potential target for vaccines, the carbohydrate coating makes it difficult or impossible for antibodies to access and neutralize it. Yet, sometimes, holes naturally appear in this coating, exposing the Env protein to potential antibodies. Zhu said he and the other researchers wanted to find a way to target these holes.
“The idea would be to do molecular surgery to copy sections of the virus’s surface and paste them onto different, benign proteins, so they would look but not act like the Env protein,” Zhu says. “Hopefully, this would allow the immune system to recognize the virus and create antibodies to neutralize it in the future.”
In the current study, the researchers used computational models to design proteins that would mimic the conserved protein surface of different strains of HIV to be used in the vaccine. Typically, proteins are engineered by changing one amino acid at a time, they wanted to try a different approach.
“Here we computationally design epitopes that mimic such surface features (carbohydrate-occluded neutralization epitopes, or CONE) of Env through ‘epitope transplantation’, in which the target region is presented on a carrier protein scaffold with preserved structural properties,” the authors write. “Scaffolds displaying the four CONEs are examined for structure and immunogenicity. Crystal structures of two designed proteins reflect the computational models and accurately mimic the native conformations of CONEs.”
“Instead of changing one amino acid at a time, it’s a large surface of the HIV strain that is cut and then plugged onto a different protein,” states Dokholyan. “It’s an important milestone be able to do these major molecular surgeries, and it’s very exciting that the strategy worked with a very high accuracy.”
After creating immunogens that used the new, HIV-mimicking proteins, the researchers immunized rabbits and drew blood samples once a month. After analyzing the samples, the researchers found that the blood contained antibodies that were able to bind onto HIV. While the research team said that the findings are encouraging, they admitted that there is still more work to be done.
“It’s important that we were able to generate an immune response to HIV and show that it’s possible as a proof of concept,” Dokholyan says. “But we still need to improve the antibodies’ neutralization abilities and other aspects before it can become a viable vaccine.”
In the future, the protein design method could potentially help create and personalize vaccines for different diseases in various areas in the world.
“Diseases can vary by location, for example, there are different strains of HIV in various countries or regions,” Dokholyan concludes. “If we can easily customize proteins for vaccines, that’s a good example of where personalized medicine is going to play a role.”