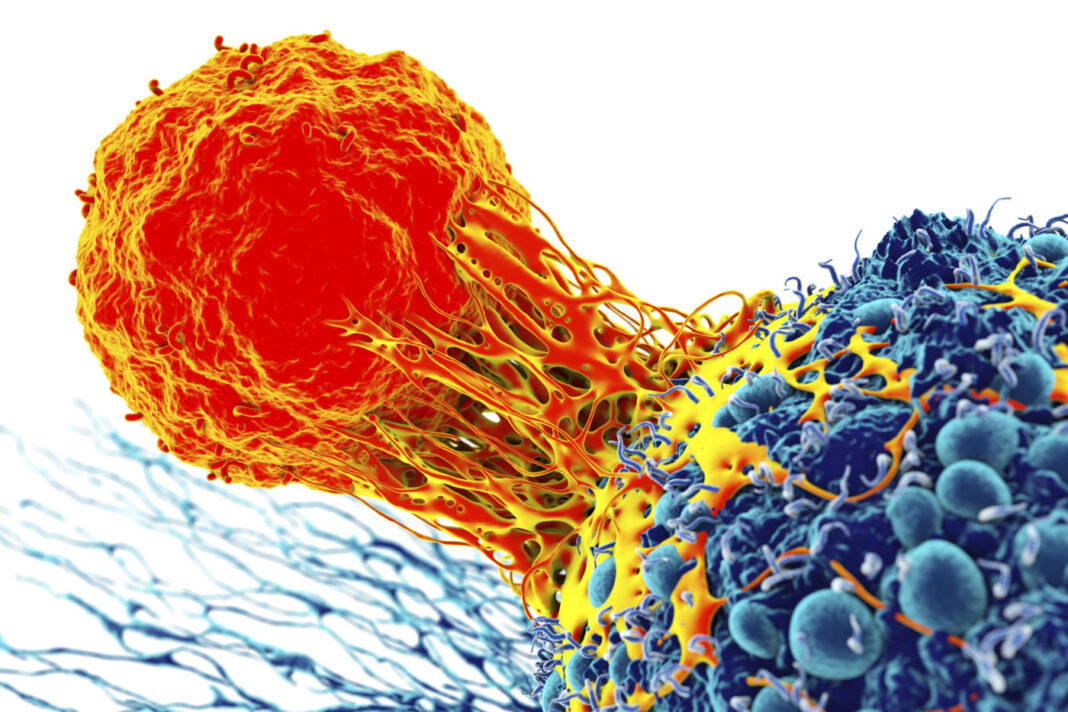
T cells engineered to kill cancer cells have had some success solving a relatively simple problem: recognizing a single cancer-associated antigen. Working at this level, T cells can sometimes target relatively simple cancers, such as hematological cancers. But solid tumors represent a more difficult problem. They are less likely to express a single antigen that clearly distinguishes them from healthy cells. To zero in on solid tumors, engineered T cells may need to recognize cells that express distinctive combinations of nonspecific antigens.
In other words, if engineered T cells are to attack solid tumors, they will need more sophisticated logic circuits. Instead of simply recognizing whether a single input is present, T cells to process multiple inputs. How? With circuitry that can handle Boolean logic.
Boolean-adept T cells are being developed by scientists based at the University of California, San Francisco (UCSF). Led by Wendell Lim, PhD, principal investigator, these scientists used in silico screening to identify multi-antigen signatures that improve tumor discrimination by CAR T cells engineered to integrate multiple antigen inputs via Boolean logic, for example, AND and NOT.
This work appeared recently in Cell Systems, in a paper titled, “Discriminatory Power of Combinatorial Antigen Recognition in Cancer T Cell Therapies.” The paper predicted that dual antigens should significantly outperform the best single clinically investigated CAR targets. The paper also described how this prediction was confirmed experimentally. Finally, the paper suggested that by recognizing triple antigen combinations, T cells could achieve close to ideal tumor-versus-normal tissue discrimination for several tumor types.
These findings have been extended in more recent work, which appeared November 26 in Science, in an article titled, “Precise T cell recognition programs designed by transcriptionally linking multiple receptors.” As did the earlier study, the more recent study used a system known as synNotch, a customizable molecular sensor that allows synthetic biologists to fine-tune the programming of cells. Developed in the Lim lab in 2016, synNotch is a receptor that can be engineered to recognize myriad target antigens. The output response of synNotch can also be programmed, so that the cell executes any of a range of responses once an antigen is recognized.
In the earlier study, the Lim team used synNotch to program T cells to kill kidney cancer cells that express a unique combination of antigens called CD70 and AXL. Although CD70 is also found in healthy immune cells, and AXL in healthy lung cells, T cells with an engineered synNotch AND logic gate killed only the cancer cells and spared the healthy cells.
In the new Science paper, the lead author of which is former UCSF graduate student Jasper Williams, multiple synNotch receptors were daisy-chained to create a host of complex cancer recognition circuits. Since synNotch can activate the expression of selected genes in a “plug and play” manner, these components can be linked in different ways to create circuits with diverse Boolean functions, allowing for precise recognition of diseased cells and a range of responses when those cells are identified.
“In this study, we engineered a diverse library of multireceptor cell-cell recognition circuits by using synthetic Notch receptors to transcriptionally interconnect multiple molecular recognition events,” wrote the authors of the Science article. “These synthetic circuits allow engineered T cells to integrate extra- and intracellular antigen recognition, are robust to heterogeneity, and achieve precise recognition by integrating up to three different antigens with positive or negative logic. A three-antigen AND gate composed of three sequentially linked receptors shows selectivity in vivo, clearing three-antigen tumors while ignoring related two-antigen tumors.”
For Lim, cells are akin to molecular computers that can sense their environment and then integrate that information to make decisions. Since solid tumors are more complex than blood cancers, “you have to make a more complex product” to fight them, he said.
“Currently, most cancer treatments, including cell therapies, are told ‘block this,’ or ‘kill this,'” he continued. “We want to increase the nuance and sophistication of the decisions that a therapeutic cell makes.”
According to Lim, his team is essentially creating a cell engineering manual for building different classes of therapeutic T cells. The manual, he asserts, could contain blueprints for engineered cells that could recognize almost any possible type of combinatorial antigen pattern.
For example, a synNotch receptor can be engineered so that when it recognizes antigen A, the cell makes a second synNotch that recognizes B, which in turn can induce the expression of a CAR that recognizes antigen C. The result is a T cell that requires the presence of all three antigens to trigger killing. In another example, if the T cell encounters an antigen present in normal tissues but not in the cancer, a synNotch receptor with a NOT function could be programmed to cause the T cell carrying it to die, sparing the normal cells from attack and possible toxic effects.
The Science paper describes how complex synNotch configurations allowed T cells to selectively kill cells carrying different combinatorial markers of melanoma and breast cancer. Moreover, when synNotch-equipped T cells were injected into mice carrying two similar tumors with different antigen combinations, the T cells efficiently and precisely located the tumor they had been engineered to detect, and reliably executed the cellular program the scientists had designed.
Lim’s group is now exploring how these circuits could be used in CAR T cells to treat glioblastoma, an aggressive form of brain cancer that is nearly always fatal with conventional therapies.
“You’re not just looking for one magic-bullet target. You’re trying to use all the data,” Lim insisted. “We need to comb through all of the available cancer data to find unambiguous combinatorial signatures of cancer. If we can do this, then it could launch the use of these smarter cells that really harness the computational sophistication of biology and have real impact on fighting cancer.”