The hidden benefits of tea are no secret. While some brews have more health advantages than others, there is plenty of evidence that shows the benefits of tea on overall health. Tea has been linked to having a positive effect on weight loss, warding off heart disease and cancer, fighting off inflammation, and lowering blood pressure. A new study from the University of California, Irvine (UCI) shows that compounds in both green and black tea relax blood vessels by activating ion channel proteins in the blood vessel wall. The new findings help explain the antihypertensive properties of tea compounds and may pave the way to the development of new blood pressure-lowering medications.
The new study is published in Cellular Physiology and Biochemistry, in a paper titled, “KCNQ5 Potassium Channel Activation Underlies Vasodilation by Tea.” The research was led by the laboratory of Geoffrey Abbott, PhD, a professor in the department of physiology and biophysics at the UCI School of Medicine and Kaitlyn Redford, a graduate student in the Abbott Lab.
Hypertension is a common condition in which the long-term force of the blood is high enough that it may eventually cause health problems, such as heart disease. Blood pressure normally rises and falls throughout the day, but it causes damage if it stays high for a long time.
“Tea, produced from the evergreen Camellia sinensis, has reported therapeutic properties against multiple pathologies, including hypertension. Although some studies validate the health benefits of tea, few have investigated the molecular mechanisms of action,” the researchers wrote.
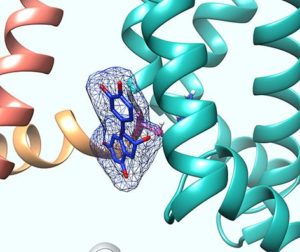
The researchers revealed that two catechin-type flavonoid compounds, epicatechin gallate (ECG) and epigallocatechin-3-gallate (EGCG), found in tea, each activate a specific type of ion channel protein named KCNQ5, which allows potassium ions to diffuse out of cells to reduce cellular excitability.
KCNQ5 is a gene encoding an important channel for neuronal function and is widely expressed in the brain and in skeletal muscle.
“We found by using computer modeling and mutagenesis studies that specific catechins bind to the foot of the voltage sensor, which is the part of KCNQ5 that allows the channel to open in response to cellular excitation. This binding allows the channel to open much more easily and earlier in the cellular excitation process,” explained Abbott.
Consumption of green or black tea has been shown to reduce blood pressure by a small but consistent amount, and now the identification of KCNQ5 as a novel target for the hypertensive properties of tea catechins may help improve current treatments.
Since catechins have the ability to cross the blood-brain barrier, this finding may help lead to new strategies and treatments for diseases related to KCNQ5 mutations.
The researchers in the present study observed that when black tea was directly applied to cells containing the KCNQ5 channel, the addition of milk prevented the beneficial KCNQ5-activating effects of tea. However, said Abbott, “we don’t believe this means one needs to avoid milk when drinking tea to take advantage of the beneficial properties of tea. We are confident that the environment in the human stomach will separate the catechins from the proteins and other molecules in milk that would otherwise block catechins’ beneficial effects.”
Using mass spectrometry, the researchers also observed that warming green tea to 35°C alters its chemical composition in a way that causes it to be more effective at activating KCNQ5.
“Regardless of whether tea is consumed iced or hot, this temperature is achieved after tea is drunk, as human body temperature is about 37°C,” added Abbott. “Thus, simply by drinking tea we activate its beneficial, antihypertensive properties.”
“KCNQ5 activation contributes to vasodilation by tea; ECG and EGCG are
candidates for future anti-hypertensive drug development,” concluded the researchers.







