Scientists at Osaka University and colleagues have revealed a correlation between the cancer cell-killing activity of T cells within tumors in lung cancer patients and this same activity in T cells located far away in the blood in these same patients. They have also shown that this level of activity in the blood correlates with the effectiveness of a commonly used medication in cancer immunotherapy.
This work (“Peripheral T cell cytotoxicity predicts T cell function in the tumor microenvironment“), published in Scientific Reports, provides a simple means of identifying which patients would benefit from cancer immunotherapy, potentially improving the outcomes of treatment for lung cancer, according to the researchers.
The team used an approach called bispecific T cell engager technology (BiTE), which ensures that T cells encounter cancer cells, to assess the intensity of cancer cell killing by these immune cells. They compared this cell killing activity of T cells from lung cancer tumors, healthy lung tissue, and peripheral blood. They also investigated the correlations of such activity with factors such as whether the patient was a smoker, the presence of certain gene mutations, and the levels of immunity-related molecules called cytokines.
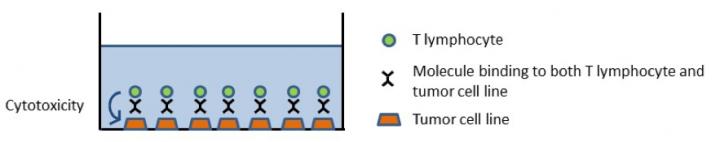
“Cancer immunotherapy, including immune checkpoint inhibitors, exerts beneficial effects in cancer patients. However, immune checkpoint inhibitors are only advantageous for a limited population of cancer patients. Therefore, companion diagnostics are needed in order to identify patients for whom these therapies are effective. In the present study, we evaluated detailed immunological aspects in clinical specimens from non-small cell lung cancer (NSCLC) patients. We analyzed the immune profiles, T cell cytotoxicity, and TCR repertoire of peripheral blood, normal lung tissue, and tumor tissue from NSCLC patients,” wrote the investigators.
“By using bispecific T-cell engager technology to assess the cytotoxicity of T cells, we found that the cytotoxicity of tumor-infiltrated T cells closely correlated with that of peripheral T cells. This correlation was supported by the immune profiles, cytokine production, and results of the TCR repertoire analysis from these specimens. We also found that the cytotoxicity of peripheral T cells has potential as a predictor of the effects of nivolumab in the tumor microenvironment. These results imply further applications to blood-based immune monitoring systems and predictive biomarkers for cancer immunotherapy.”
“After optimizing the BiTE conditions for assaying T cell cytotoxicity, we characterized the T cells from the three sample sets and looked at their correlations with other clinical and lifestyle-related factors,” explained Atsushi Kumanogoh, MD, PhD, principal investigator at the Immunology Frontier Research Center of Osaka University. “We first found that T cells were more cytotoxic in smokers and that high T cell cytotoxicity within tumors was linked to the expression of some cytokines.”
The team then found that, within individual patients, the cytotoxicity of T cells in the blood was actually the factor that most strongly predicted the cytotoxicity of T cells within lung tumors. It also reflected the effectiveness of the immune checkpoint inhibitor nivolumab at destroying tumor cells. This inhibitor is an antibody that targets and blocks the activity of the molecule PD-1 in suppressing the immune system.
“The ability to diagnose cases using just blood samples would mean that patients won’t have to undergo invasive procedures such as biopsy for tumors in the lungs,” lead author Kota Iwahori, MD, PhD, said. “We could then evaluate whether the use of cancer immunotherapy would be appropriate for a particular patient, hopefully improving the outcomes in lung cancer patients.”






