The National Institute of Allergy and Infectious Diseases says that the list of emerging infectious diseases is hardly limited to outbreaks of previously unknown pathogens. It also includes known diseases that gain in numbers or geographic extent, or that persist and remain uncontrolled. The list includes chikungunya, HIV, and dengue infections as well as the reappearing influenza and pneumococcal diseases. Industry, government, and academia are attempting to stay one step ahead of these diseases by developing new vaccines, technologies, and therapeutics. This article describes some of these creative approaches and emphasizes the contributions of industry players.
Because viruses often mutate, some new vaccines are targeting updated serotypes currently in circulation. For example, an earlier pneumococcal vaccine targeted serotypes responsible for about 4% of today’s adult illness, while a new vaccine in clinical trials targets serotypes responsible for 85%. Another strategy for vaccine development is to employ several platforms. One company is utilizing two approaches: a large vector-based vaccine and a virus-like particle (VLP). The former can incorporate elements that encode different viral proteins. The latter can incorporate structures that allow it to mimic wild-type viruses.
Other vaccine developers are interested in countering the increasing danger of antibiotic-resistant bacteria. For example, vaccines are being built that incorporate multiple inactivated staphylococcus toxins.
Besides developing innovative technologies, industry players are collaborating with government entities. For example, Johnson & Johnson Innovation—JLABS has launched Blue Knight, a collaboration with the Biomedical Advanced Research and Development Authority (BARDA), part of the Administration for Strategic Preparedness and Response at the U.S. Department of Health and Human Services.
Invasive pneumococcal disease
The medical history is long on humans and Streptococcus pneumoniae, or pneumococcus, yet new chapters continue to be written on treating the disease in both children and adults. Although pneumococcus is commonly a part of the oral microbiome, it also has the potential to become a deadly pathogen, especially in infants, young children, and older adults. Pneumococcal diseases range, for example, from sinusitis to life-threatening pneumonia, sepsis, or meningitis.
“Pneumococcus has been responsible for an enormous amount of disease consistently, and vaccines have been the way we have reduced that public health disease burden,” stresses Heather Platt, MD, distinguished scientist, Merck. “Considering pneumococcus as an emerging disease is appropriate because the pathogen still imposes an important unmet disease burden in adults.”

Merck
The first pneumococcal vaccines in 1909 used whole cells, and contemporary vaccines often target its serotype-specific polysaccharide coat. Coupled with a nontoxic carrier protein, such polysaccharide conjugate vaccines (PCVs), however, protect against only the specific serotypes incorporated. “Over time, the serotypes differ,” Platt notes. “For example, PCV7 was the first conjugate vaccine. Yet today, the serotypes in that vaccine are responsible for only about 4% of adult disease in the United States.”
Merck’s current 21-valent candidate, V116, includes 8 serotypes not in any currently licensed PCV. Platt elaborates, “V116 was designed to specifically look at what serotypes are causing disease. While some of those are in current vaccines, other serotypes are not.
“We have examined epidemiology in the United States and major countries that have good surveillance systems, and we’ve taken that as part of the way to design an improved vaccine. The serotypes in V116 are responsible for about 85% of adult disease. That is a substantial jump. We are excited that this vaccine has the potential to have a really positive public health impact.”
The vaccine candidate, currently in Phase III trials, should provide readouts before the end of the year. Merck is also focusing on other programs in areas of high interest such as dengue and respiratory syncytial virus (RSV). Platt concludes, “We continue our investments in exploring how to develop and use vaccines that examine specific populations of people who will benefit.”
Multiple approaches
With a host of potential disease threats on the horizon, how do companies choose which to pursue? Paul Chaplin, PhD, president and CEO, Bavarian Nordic, highlights several considerations: “It’s all about people and patients with unmet medical needs in an area that needs a new or improved vaccine. Additionally, we consider if we have a scientific approach likely to work, or even a potentially different platform to which we can gain access. Of course, it is also important to develop public and private partnerships to fund such projects.”

Bavarian Nordic
Bavarian Nordic is focusing on several targets and using multiple approaches. In one program, the company is employing its proprietary platform, MVA-BN, whose basis is a nonreplicating, modified vaccinia Ankara (MVA) vector–based vaccine. The company is using this platform to advance an RSV vaccine (MVA-BN-RSV)—currently the subject of a Phase III trial—and several other programs, including one for an approved smallpox/monkeypox vaccine.
“MVA has several benefits,” Chaplin explains. “For example, it can incorporate a larger number of encoded viral proteins. The RSV vaccine incorporates five different RSV antigens. Further, MVA not only generates antibodies, but it also stimulates T cells. We believe that for some diseases, including RSV, this is quite important.”
The company is also working on a vaccine against chikungunya virus, CHIKV, an ongoing public health threat that can cause severe and debilitating symptoms including rash, fever, and arthralgias (joint pain). Currently unopposed by any vaccine or treatment, CHIKV has been found in more than 100 countries, and it is emerging in previously unaffected areas, including those often visited by travelers. The two main mosquitoes that transmit the viruses (Aedes aegypti and Aedes albopictus) have been expanding their habitat range—a change attributed to climate change as well as modern shipping and transportation.
The first vaccine for CHIKV could come from Bavarian Nordic, which has an adjuvanted VLP-based vaccine candidate in Phase III testing. Although the CHIKV VLP is structured nearly identically to a wild-type virus, it cannot replicate because no viral genetic material is incorporated. “This is a very efficient way for B cells to produce antibodies,” Chaplin asserts. “The VLP works well for generating a strong and lasting antibody response against the virus and has an excellent safety profile.” The company expects to complete the Phase III study this year.
Structure-guided design
There’s little need to wonder what AbVacc does. The company makes that clear with its admirably descriptive name: “Ab” stands for antibodies, and “Vacc” stands for vaccines. AbVacc’s president and chief scientific officer, Javad Aman, PhD, points out that the company’s antibody development programs and vaccine development programs are mutually integrated. “Our aim,” he emphasizes, “is to both prevent and/or treat a variety of infectious diseases.”
AbVacc leverages structural information about protective and distractive/decoy epitopes to design novel immunogens that focus the immune response on the protective epitopes, and that blunt the immune responses to the nonprotective epitopes. The company also extends its rational vaccine development work to antibody discovery. For example, the company leverages Smart Immunogens to serve as Smart Probes that interrogate the immune repertoire of humans and vaccinated macaques. Doing so allows AbVacc to identify the best antibodies, excluding undesirable antibodies in the discovery process and finding the low-frequency, high-value monoclonal antibodies (mAbs).
The company has developed a Staphlococcus aureus (SA) vaccine called IBT-V02. It is a five-component, rationally designed toxoid vaccine. (A toxoid is a chemically or heat-inactivated toxin.)
IBT-V02, which covers about 15 different SA toxins, was evaluated in preclinical studies for its ability to prevent acute skin infections of SA, as well as to protect against subsequent infections.
“Immunization of mice and rabbits with IBT-V02 generated antibodies with strong neutralizing activity against toxins included in the vaccine, as well as cross-neutralizing activity against multiple related toxins, and protected against skin infections by several clinically relevant SA strains,” Aman and colleagues reported in Frontiers in Immunology (2021; 2: 624310). “Efficacy of the vaccine was also shown in non-naïve mice pre-exposed to SA. Furthermore, vaccination with IBT-V02 not only protected mice from a primary infection but also demonstrated lasting efficacy against a secondary infection.”
SA is one of the most common pathogens in healthcare and community settings. It can cause a wide range of diseases and outcomes from minor skin irritations to invasive infections, sepsis, and death. Both methicillin-resistant and multidrug-resistant strains are emerging, making a difficult situation even worse. Although multiple candidate vaccines have been tested in clinical trials, none of them has been efficacious.
Aman hopes to break that losing streak: “We expect to enter clinical trials later this year. Our next steps after Phases I and II are completed would be to assess the vaccine in HIV patients, diabetics, and the pediatric population. For children susceptible to SA, a vaccine administered early in life could lead to a lifetime buildup of immunity.”
Leveraging its SA antigen development, the company is working on a mAb cocktail against SA bacteremia. The cocktail could serve as an adjunct to surgical procedures, or as a treatment for SA infections associated with prosthetic devices. “We collaborate with EliteImmune to identify the optimal mAb cocktail that can be given as a treatment,” Aman says. “And then we introduce mutations to increase the mAb half-life and extend the therapeutic value.”
The company is also conducting research programs to pit its mutually integrated approach against an array of targets. These include Ebola virus, Marburg virus, Nipah virus, influenza viruses, Clostridium difficile, and Bacillus anthracis.
The Blue Knight program
“Anticipate, Activate, Amplify.” Those words describe the quest of the Blue Knight program, a collaboration between Johnson & Johnson Innovation—JLABS and BARDA. Blue Knight is designed to create opportunities for early-stage companies to develop next-generation technologies, vaccines, and therapeutics. When Blue Knight launched in August 2020, it had seven companies in its portfolio. Today, the program includes 37 companies.
“Blue Knight supports early-stage companies that are strategically aligned to both Johnson & Johnson and BARDA,” says Rachel Rath, director of the BARDA Alliance at Johnson & Johnson Innovation—JLABS. She adds that for the most part, these companies have expertise in emerging infectious diseases and in enabling technologies for next-generation therapeutics and vaccines.

Johnson & Johnson—JLABS
Rath notes that the technologies include (but are not limited to) those that could facilitate early detection, clinical trial diversity and enrollment, and manufacturing and distribution. She explains, “Companies may have access to space within JLABS, fee assistance for access to JLABS residency, mentorship from the Johnson & Johnson family of companies and BARDA, equipment at select JLABS locations, and dedicated programming and engagement opportunities.”
Rath notes the application for Blue Knight is open to early-stage companies that can apply on a rolling basis. She summarizes, “We hope to help support next-generation technologies so that we can more rapidly address emerging threats in the future through detection, prevention, and treatment approaches.”
Broad-spectrum attack
With respect to emerging infectious diseases, the holy grail of vaccine and therapeutic development is to achieve broad coverage. Those seeking this object include Centivax, a recent awardee of the Blue Knight program. The company’s co-founder and CEO, Jacob Glanville, PhD, explains the importance of broad coverage as follows: “Many pathogens evolve and mutate rather quickly, causing vaccines to become rapidly obsolete. For example, even updated vaccines, such as the flu vaccine, can be ineffective by the time the flu season comes around.”

Centivax
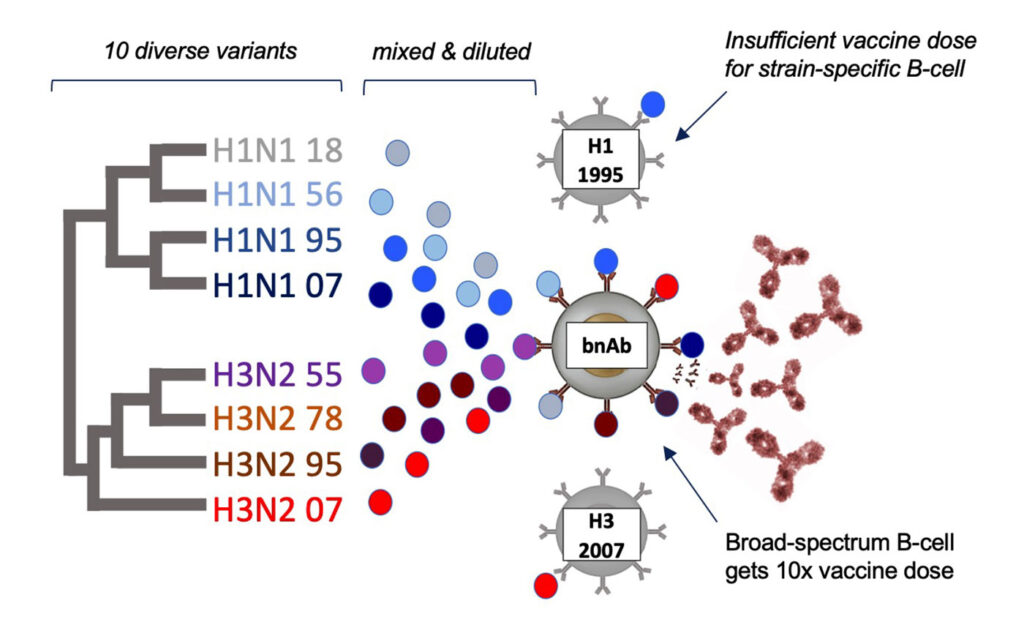
Glanville believes that focusing on a pathogen’s conserved sites is the key. “If you can focus on conserved sites that don’t often mutate, you can create a more universal vaccine,” he says. “However, it turns out to be very difficult to target these sites since they are non-immunodominant.”
The company overcomes this challenge by applying “Computational ImmunoEngineering.” Glanville elaborates, “We use computational methods to select—and in many cases design—a library of natural and synthetic variants of a pathogen target protein. The library contains many diverse combinations of mutations that we know are tolerated on the protein, but they all share at least one conserved site that the pathogen cannot mutate.” The company then identifies the best 8–18 candidates and formulates a vaccine for injection.
“A vaccine will typically induce more than 100 different antibodies,” Glanville points out. “Our technology causes those 100 antibodies to target the conserved sites on the pathogen, essentially creating a 100-valent broad-spectrum multidrug cocktail that your own body produces after being vaccinated.”
In some cases, these vaccine-elicited, broadly neutralizing antibodies can themselves be isolated and used as mAb therapeutics. The company capitalizes on the production of these antibodies again using its immunoengineering capability. “Bioengineering of antibodies helps us to enhance the properties of antibodies such as thermostability and extended half-life,” Glanville notes. “These advances will help transform access to biologic medicine for patients globally.”
The company’s portfolio currently consists of vaccine candidates in preclinical development. The most advanced candidate, an influenza vaccine, is scheduled to graduate to clinical trial production toward the end of 2024. Glanville anticipates that in the near future, emerging infectious diseases could be countered by emerging Centivax vaccines. “There are over 25 pathogens that we could uniquely address with our broad-spectrum vaccine platform,” he declares. “We are in vivo with Centi-Flu (influenza), Centi-COV (coronaviruses), and Centi-HIV programs.” He expects that there will be additional programs, including vaccines for dengue virus, Zika virus, Ebola virus, Marburg virus, human papilloma virus, and herpes virus, as well as a combination broad-spectrum flu/COVID-19/RSV vaccine.”


