By tweaking the structure of the antifungal drug amphotericin B (AmB), researchers at the University of Illinois Urbana-Champaign and collaborators at the University of Wisconsin-Madison have generated a new molecule, dubbed Am-2-19, that they suggest has the potential to harness the power of AmB against fungal infections, but without the associated kidney toxicity.
“This molecule is kidney-sparing, it is resistance evasive, and it has broad spectrum efficacy,” said University of Illinois Urbana-Champaign researcher Arun Maji, PhD, co-first author of the team’s published paper in Nature. “We tested this molecule against over 500 different clinically relevant pathogen species in four different locations. And this molecule completely surprised us by either mimicking or surpassing the efficacy of current clinically available antifungal drugs.” Maji and colleagues reported on the development and testing of Am-2-19 in a paper titled, “Tuning sterol extraction kinetics yields a renal-sparing polyene antifungal.”
Amphotericin B, a naturally occurring small molecule compound produced by bacteria, is used as a last resort drug to treat fungal infections. While AmB excels at killing fungi, it is reserved as a last line of defense because it also is toxic to the human patient—and particularly the kidneys.
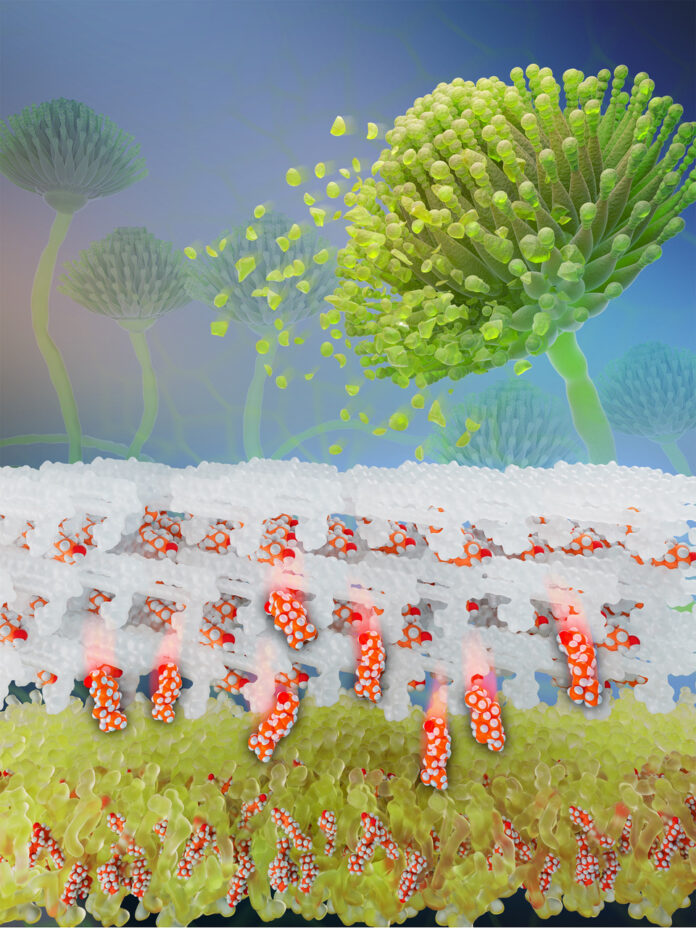
![The mechanism for a critical but highly toxic antifungal is revealed in high resolution. Self-assembled Amphotericin B sponges rapidly extract sterols from cells. This atomic level understanding yielded a breakthrough kidney-sparing antifungal agent. [Jose Vazquez]](https://www.genengnews.com/wp-content/uploads/2023/11/AmB_sterol_sponge-1-225x300.jpeg)
“Fungal infections are a public health crisis that is only getting worse,” said research lead Martin D. Burke, MD, PhD, a professor at the University of Illinois and the Carle Illinois College of Medicine. “And they have the potential, unfortunately, of breaking out and having an exponential impact, kind of like COVID-19 did.”
Burke’s group has spent years exploring AmB, with a view to making a derivative that can kill fungi without harm to humans. “… let’s take one of the powerful tools that nature developed to combat fungi and turn it into a powerful ally,” he said.
In previous studies, the researchers had developed and leveraged a building block-based approach to molecular synthesis and teamed up with a group, led by Chad Rienstra, PhD, a professor at the University of Wisconsin-Madison, specializing in solid-state nuclear magnetic resonance. Together, the teams uncovered the mechanism by which AmB kills fungi, by acting like a sponge to extract ergosterol from fungal cells. “Decades of previous efforts to develop renal-sparing polyene antifungals were misguided by the classic membrane permeabilization model,” they explained. “Recently, the clinically vital but also highly renal-toxic small-molecule natural product amphotericin B was instead found to kill fungi primarily by forming extramembraneous sponge-like aggregates that extract ergosterol from lipid bilayers.”
For their new work, the two groups again worked together to find that AmB similarly kills human kidney cells by extracting cholesterol, the most common sterol in people. “Cholesterol extraction was found to drive the toxicity of amphotericin B to human renal cells,” they wrote. The researchers then resolved the atomic-level structure of AmB sponges when bound to both ergosterol and cholesterol. “The atomic resolution models were really the key to zoom in and identify these very subtle differences in binding interactions between AmB and each of these sterols,” said Illinois graduate student and co-first author Corinne Soutar.
Armed with the information from the NMR studies, the Illinois team began synthesizing and testing derivatives with slight changes to the region that binds to ergosterol and cholesterol, while also boosting the kinetics of the ergosterol-removing process to maintain efficacy. “Using this structural information along with functional and computational studies, we achieved a significant breakthrough in understanding how AmB functions as a potent fungicidal drug,” Rienstra said. “This provided the insights to modify AmB and tune its binding properties, reducing its interaction with cholesterol and thereby reducing the toxicity.”
Enabled by collaborators and facilities at the Carl R. Woese Institute of Genomic Biology and the University of Illinois veterinary clinical medicine professor Timothy Fan, PhD, the researchers tested the most promising derivatives—first with in vitro assays, quickly assessing the efficacy in killing fungi, then moving to cell cultures and eventually live mice, assessing toxicity.
![The researchers put promising candidates through extensive testing for efficacy and toxicity, both in vitro and in vivo. Pictured, from left: Arun Maji, Agnieszka Lewandowska and Corinne Soutar. [Michelle Hassel, University of Illinois.]](https://www.genengnews.com/wp-content/uploads/2023/11/burke-group230929-mh-013-m-1-300x200.jpeg)
The authors explained, “Our examination of high-resolution structures of amphotericin B sponges in sterol-free and sterol-bound states guided us to a promising structural derivative that does not bind cholesterol and is thus renal sparing.” However, this initial derivative was also less potent because it extracts ergosterol more slowly,” they continued. “Selective acceleration of ergosterol extraction with a second structural modification yielded a new polyene, AM-2-19 …”
The researchers evaluated AM-2-19 in human blood and kidney cells to screen for toxicity, and carried out experiments with AM-2-19 in mouse models of three common, stubborn fungal infections, which confirmed that the molecule was highly efficacious. AM-2-19, they stated, “… is renal sparing in mice and primary human renal cells, potent against hundreds of pathogenic fungal strains, resistance evasive following serial passage in vitro, and highly efficacious in animal models of invasive fungal infections.”
Burke commented, “This work is a demonstration that, by going deep into the fundamental science, you can take a billion-year head start from nature and turn it into something that hopefully is going to have a big impact on human health. During my medical rotations, we called AmB ‘ampho-terrible,’ because of how hard it was on patients … Decoupling the efficacy from the toxicity turns ‘ampho-terrible’ into ‘ampho-terrific.’ We are very excited about the potential we are seeing, although clinical study is needed to see if this potential translates to people.”
The authors concluded, “Thus, advanced understanding of the mechanism by which polyene macrolide natural products kill fungal and human cells enabled the selective tuning of sterol extraction kinetics to yield a new polyene antifungal that is both renal sparing and highly potent in clinically relevant animal models of invasive fungal infections.”
AM-2-19 has been licensed to Sfunga Therapeutics—which partly supported the work, and in which Burke has an equity interest—and recently entered Phase I clinical trials.