Organoids may make the truest tissue models. But what makes the truest organoids? An answer to that question was suggested in a review article that appeared 10 years ago,1 just a few years after organoids began incorporating induced pluripotent stem cells. Today, the review article’s main point is as apt as ever: “Organoids are derived from pluripotent stem cells or isolated organ progenitors that differentiate to form an organ-like tissue exhibiting multiple cell types that self-organize to form a structure not unlike the organ in vivo. … Because organoids can be grown from human stem cells and from patient-derived induced pluripotent stem cells, they have the potential to model human development and disease. Furthermore, they have potential for drug testing and even future organ replacement strategies.”
Organoids of this sort can mirror the genotype and phenotype of real tissues. Indeed, this capability has been demonstrated in the creation of organoids that mimic different tissues, such as tissues of the brain, gut, and lung. Also, there are immune organoids, or lymphoid tissue models. (Alternatively, the term “immune organoids” may refer to tissue models of any type that incorporate a functional immune system.)
Organoid development has been accelerating thanks to the introduction of commercial technologies. For example, there are extracellular matrix gels that, in the words supplied by the review, allow organoids to “self-organize through cell sorting out and stem cell lineage commitment in a spatially defined manner to recapitulate organization of different organ cell types.” Also, there are technologies that combine organoids with microfluidic systems, which can provide sophisticated microenvironments for recapitulating body organs.
Such technologies are enabling the modeling of rare diseases and tumors. Also, they are encouraging developers and regulators to position organoids as alternatives to animal models in drug testing. It should come as no surprise, then, that organoids represent a market with enormous growth potential. According to a market research study issued in 2023 by Insight Partners, the organoid market will register an annual growth rate of 22% in the coming years and reach a value of $12 billion by 2030.
Mini organs on scaffolds
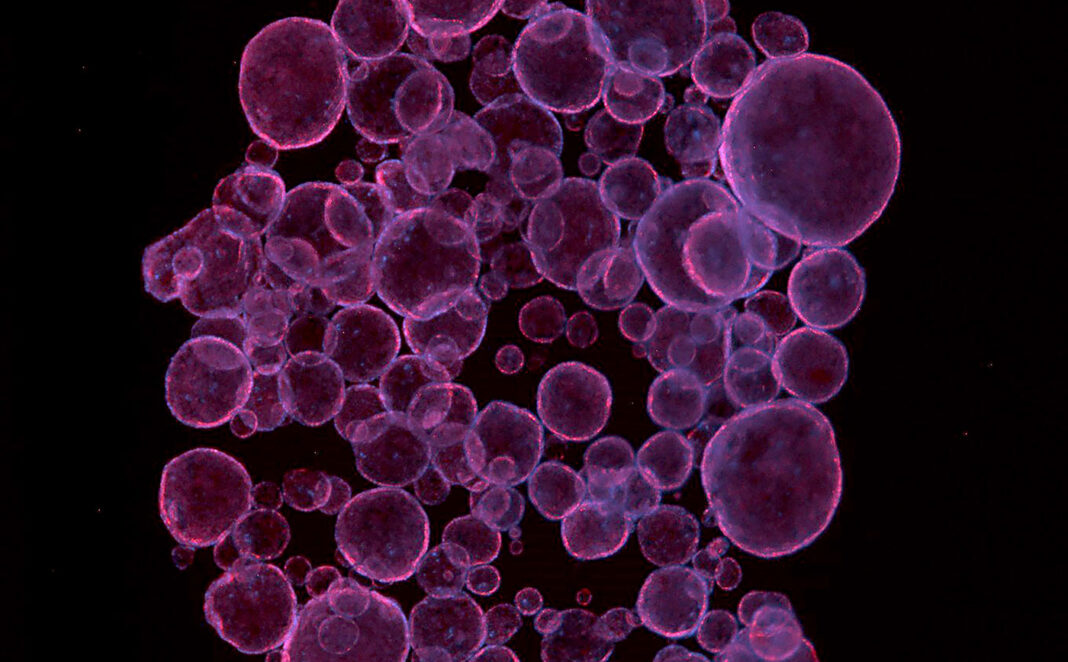
“Organoids have become increasingly popular as tissue models since they can retain the genetic and phenotypic heterogeneity of the original tissue,” reports Hilary Sherman, senior applications scientist, Corning Life Sciences. “This concept has become invaluable for cancer research, where we know that individuals with similar cancers can respond very differently to drugs. Additionally, organoid models can be developed more quickly and cheaply than animal models.”
Sherman notes that organoids can model diseases that are a result of multiple or varied mutations. Indeed, organoids can model complex genetic diseases such as cancer. If organoids incorporate patient-specific mutations, individualized modeling is possible. Such modeling could be used to determine which drugs would be most suitable for individual patients.

Corning Life Sciences
Organoids can be assembled or allowed to self-assemble. In either case, they are typically cultured with specific growth factors and extracellular matrix proteins. This approach was pioneered in 2009, when researchers generated the first 3D organoid culture from adult stem cells.2 They used Corning Matrigel Matrix, a solubilized basement membrane preparation. Rich in extracellular matrix proteins such as laminin and collagen, Matrigel Matrix is used to produce hydrogels that support organ/tissue architectures. Sherman comments, “Corning Matrigel Matrix is considered the gold standard hydrogel for organoid applications.”
Corning also provides the Matribot bioprinter. It is designed to print with temperature-sensitive inks, such as inks containing Matrigel matrix or collagen. “Due to the bioprinter’s temperature-controlled print head, Matrigel Matrix/organoid ink solutions can easily be dispensed into microplates,” Sherman notes. “Often, organoid assays are conducted by dispensing small droplets of Matrigel Matrix/organoid solutions onto microplates.”
“I foresee the continued development of more complex organoid models that will continue to better recapitulate what is happening in vivo,” Sherman declares. “For me, a major accomplishment would be for organoids to completely replace animal testing.”

Multiple modalities
“[Organoids] have been harnessed for a multitude of purposes,” says Dan Rocca, PhD, research leader, Charles River Laboratories. “Brain organoids, for instance, have been used not only to understand early brain development in humans, but also to study how it may have been different in our Neanderthal cousins. Lung organoids have been used to test novel antivirals against SARS-CoV-2 during the pandemic. Tumor organoids, originating from a number of tissue-restricted primary cancers, have been used to help us to reveal how therapeutics impact tumor growth.”
Rocca observes that organoids “better mimic the complexity and heterogeneity of human tumors compared to cell lines isolated from tumor biopsies and support a personalized medicine approach.” Another advantage of organoids, Rocca points out, is that they can be used to help us reduce the number of animals used in drug development.

Charles River Laboratories
However, Rocca says one current challenge is that many organoids represent an early developmental state of an organ and can often form in an inside-out manner that doesn’t always reflect the mature tissue. “They lack vascularization and relevant microenvironments, plus their cross-talk with other organs is limited,” he points out. “These problems need to be carefully considered when interpreting findings from drug screens,
for example.”
Louise Brackenbury, PhD, science director, Charles River Laboratories, indicates that most of the company’s initial organoid focus is on “generating tissue-specific safety/toxicity models to better predict downstream clinical liabilities and de-risk discovery programs early, but they can also be used for mechanism-of-action studies and for efficacy testing.”

Charles River Laboratories
Brackenbury reports that gut organoids are the most developed organoid capability within the company: “They offer better predictivity following infection with enteroviruses and allow efficient and robust screening of antivirals.”
“Alongside this,” she continues, “our immune organoids have proven suitable for testing novel immunomodulators in B-cell recall responses, which we quantify by determining antibody production. Naïve responses to novel antigens, such as Ebola glycoprotein, are detectable in some donors, suggesting it may be a suitable platform in which to determine the immunogenicity of vaccine candidates in a fully ‘human’ system.”
Looking into future possibilities of the technology, Rocca projects, “A measure of great success of the technology would be to use organoids as therapeutic tools, instead of just models. The ability to expand scalable ‘organs’ in vitro and functionally transplant these into patients to ameliorate tissue defects would be a boon for regenerative medicine.”
Large-scale production
“The top three issues I see in organoid R&D today are scalability, reproducibility, and the ability to reflect genetic diversity,” states Shantanu Dhamija, PhD, vice president, strategy and innovation, Molecular Devices, an operating company of Danaher Corporation. He believes that solving these problems will require working in collaboration with others.

Molecular Devices
“Organoid research is a team sport where collaborations are key,” Dhamija stresses. “Under Danaher’s Beacon program, we identify leading innovators in the field to fund product-driven pioneering scientific research. The latest Beacon program with Cincinnati Children’s Hospital Medical Center focuses on preclinical drug safety issues and major causes of drug failure in clinical trials.”
In early February, the organizations launched a multiyear collaboration specifically aiming to improve liver organoid technology as a drug toxicity screening solution. The project will employ technology from Molecular Devices, such as the company’s new CellXpress.ai Automated Cell Culture System. Dhamija says this is “an artificial intelligence–enabled solution for the streamlined, reliable, and reproducible production of organoids at scale.”
Dhamija notes that more than 20% of all clinical trials fail due to liver toxicity. “Despite extensive and multifaceted safety testing for pharmaceuticals, drug-induced liver injury (DILI) remains a major challenge,” he continues. “It is not reliably predicted by current in vitro models, such as immortalized cell lines or primary cells. However, liver organoids represent more highly complex, multicellular, and physiologically relevant models capable of predicting individual patient reactions to therapeutics.”
Large-scale production has been a major challenge impeding the advance of organoids into this arena. “Due to their complexity, liver organoids have been harder to produce at scale with sufficient genetic diversity for accurate analyses,” Dhamija explains. “With our new systems, we can enable the creation of more diverse liver organoids at scale. This allows better patient stratification and higher reproducibility in clinical trials.”
Better together
Cellular models often can lack the complexity and sophistication necessary for accurate translation to human physiology and disease. Emulate places combinations of human organoids and/or other cell subsets on a chip to mirror organ responses more exactly. “The chips are agnostic to the cell,” says Lorna Ewart, PhD, the company’s CSO. Cell subsets can be organoids, cell lines, primary cells, or stem cells. “The benefit of an organoid,” she note, “is that it recapitulates epithelial biology.”

Emulate
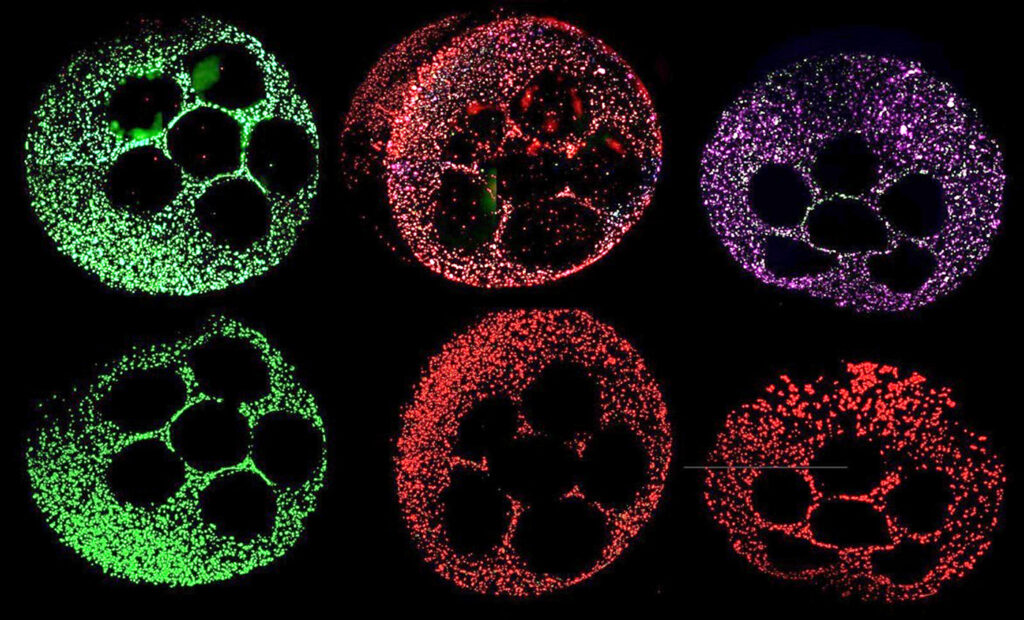
Emulate’s chip system includes an upper and a lower channel separated by a porous membrane coated with a tissue-specific extracellular matrix. To create the intestinal chip, the company begins by establishing epithelial-like organoids from endoscopic biopsies of healthy adults. These are then dissociated and seeded into the chip’s top channel. Primary microvascular endothelial cells are added to the bottom channel.
“We include an endothelial cell because communication between the epithelium and endothelium is very important,” Ewart elaborates. “We also include a cyclic stretch to emulate in vivo peristaltic motions.” Two examples of the company’s Organ-Chips that employ organoids are the Colon Intestine-Chip and the Duodenum Intestine-Chip.
Ewart reports, “We have found that when tissue-specific microenvironments are recreated, biological processes related to intestinal maturation are enhanced.” Following growth and differentiation of the cells, the intestinal chip can be utilized for drug testing, studies of inflammation, studies of tumor invasion, and other applications.
The combination of organoids and organ chips can provide the best of both worlds. “The organoid cell cultures are more complex because they have the epithelial cells, and the cell communication avenues and microenvironments allow the cells to behave as if they were inside the human body,” Ewart says. “We are leveraging the strength of both technologies.”
Emulate is also engaged in a broader narrative of building a framework to help people understand the predictive value that Organ-Chip models can generate. “More published examples of Organ-Chip characterization are required to drive wider adoption in the pharmaceutical industry and to gain acceptance by regulatory bodies,” Ewart notes.
To that end, Ewart and Daniel Levner, PhD, Emulate’s CTO, co-authored a paper that detailed workflows for the practical use of the company’s Liver-Chip.3 In another paper, Ewart and colleagues discussed the Liver-Chip’s value in predictive toxicology.4 They argued that the platform would allow manufacturers to bring safer, more effective medicines to market in less time and at lower costs.
Ewart notes that the predictive toxicology paper ranks in the top 1% of research articles of a similar age in the field. “For a scientist, that is tremendous,” she declares. “It indicates that the information is well received, widely read, and frequently referenced!”
Ewart says that Emulate’s work is particularly relevant in light of the FDA Modernization Act 2.0. Passed in 2022, the act eliminates the requirement for mandatory animal testing before a drug can begin Phase I trials. Alternatives such as cell-based assays are now acceptable, paving the way for the use of organoids. Additionally, a further update, version 3.0, is currently being considered.
Future directions
Finally, it just may be true that the future of organoid R&D is out of this world! NASA’s Expedition 71 astronauts will be conducting organoid research aboard the International Space Station’s microgravity laboratory. Although organoids have been examined in space before, the organoids that will be part of Expedition 71 will be the first organoids in space to incorporate induced pluripotent stem cells from Alzheimer’s patients. Experiments with these organoids may provide insights into mechanisms of aging, potentially identify new targets involved in neurodegenerative diseases, and help accelerate drug discovery.
Summing up the potential of the field, Hans Clevers, MD, PhD, a pioneer in organoid research and head of Roche’s Pharma Research and Early Development (pRED) notes in a blog post5 that “One can implement human organoids at every step of the way—from target identification and target validation through preclinical safety and efficacy to stratification in clinical trials.” He foresees that organoid technology “might not only revolutionize the way we do research and develop medicines, but also [enable the discovery of] completely new molecules for devastating diseases.”
References
1. Lancaster MA, Knoblich JA. Organogenesis in a dish: Modeling development and disease using organoid technologies. Science 2014; 345(6194): 1247125.
2. Sato T, Vries RG, Snippert HJ, et al. Single Lgr5 stem cells build crypt-villus structures in vitro without a mesenchymal niche. Nature 2009; 459(7244): 262–265.
3. Levner D, Ewart L. Integrating Liver-Chip data into pharmaceutical decision-making processes. Expert Opin. Drug Discov. 2023; 18(12): 1313–1320.
4. Ewart L, Athanasia Apostolou A, Briggs SA, et al. Performance assessment and economic analysis of a human Liver-Chip for predictive toxicology. Commun. Med. 2022; 2(154): 1–16.
5. Roche launches the Institute of Human Biology to pioneer new approaches for drug discovery and development. Modeling the Future blog. Published May 4, 2023. Accessed March 1, 2024.