For many patients diagnosed with cancer, hair loss is often an inevitable consequence of various therapeutic interventions. Yet, what if instead of worrying about trying to abolish the negative hair loss side-effect of cancer therapies, scientists were able to exploit hair-loss genetics to improve the new wave of immunotherapy compounds. Well, that is exactly what a group of investigators at Columbia University Irving Medical Center (CUIMC) have accomplished. Findings from the new study, published recently in Cell Systems through an article titled “IKZF1 Enhances Immune Infiltrate Recruitment in Solid Tumors and Susceptibility to Immunotherapy”, showed that a gene associated with an autoimmune form of hair loss called alopecia areata could be exploited to improve cancer immunotherapy.
“While immunotherapies have shown great promise in cancer, most patients do not benefit from these treatments because their tumors are able to evade the immune system,” explained senior study investigator Angela Christiano, Ph.D., professor of dermatology and genetics and development at Columbia University Vagelos College of Physicians and Surgeons. “But one way around this obstacle is to harness genes that cause the recruitment of T cells in autoimmune disease and use them to attract T cells to kill tumors. In this study, we showed that a gene that recruits T cells in alopecia areata, a condition in which immune cells attack and destroy hair cells, is turned off in various types of cancer, protecting them from the immune system. But if we turn that gene back on, we can make those cancers vulnerable to the immune response.”
The research team began their investigation with the recognition that autoimmune diseases and cancer represent opposite ends of the immune signaling spectrum. When the immune system is overactive, a patient may be at risk for autoimmune disease; when it's underactive, cancer can evade the immune system and progress.
“We should be able to identify genetic signals that are hyperactive in autoimmune disease, and then harness those signals in tumors that have developed a way to avoid the immune response,” noted lead study investigator James Chen, Ph.D., precision medicine fellow at CUIMC.
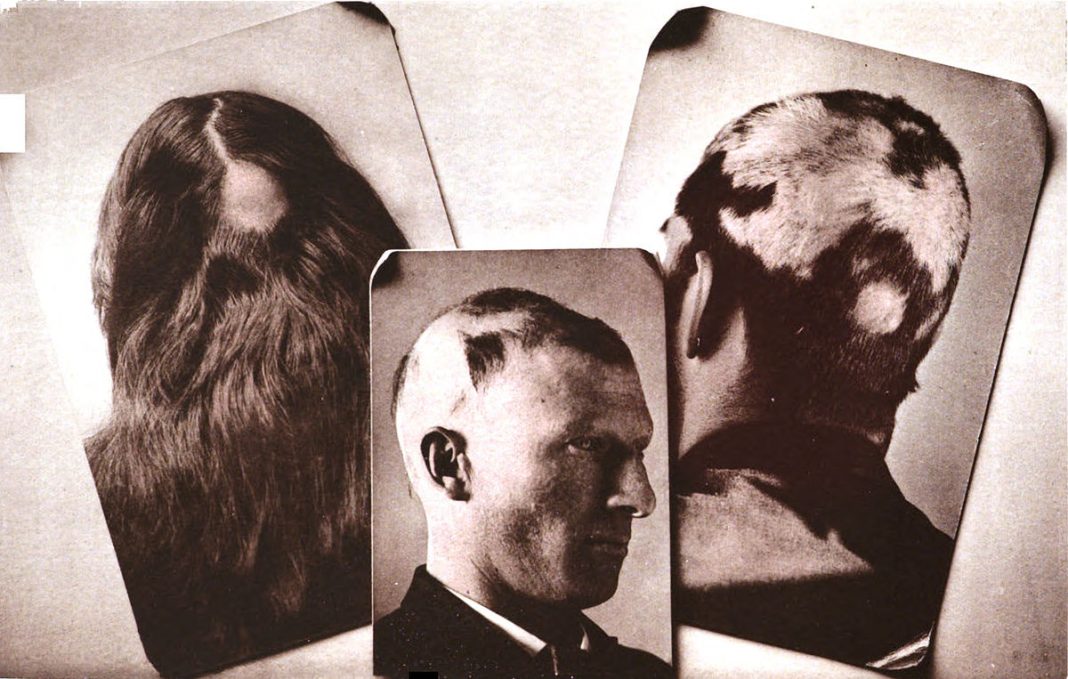
Interestingly, the research team previously identified such a genetic signal—a gene called named IKZF1—in alopecia areata. In this condition, an overactive IKZF1 gene leads to overproduction of immune cells, killing the hair follicles.
The key immune cells in alopecia areata are the same cells that many cancers can evade. These so-called killer T cells are crucial for the success of cancer immunotherapies,” remarked Dr. Christiano.
In the current study, the researchers investigated whether they could activate IKZF1 in tumor cells to attract T cells to tumors, mobilizing them to attack the cancer. Using an algorithm designed by Dr. Chen, the researchers screened genomic and bioinformatic data on thousands of cancer patients in the Cancer Genome Atlas, searching for tumor types that had IKZF1 in their regulatory networks. The algorithm predicted several types of cancer, including melanoma, that would be amenable to targeted immunotherapy, and two types that would not.
“We were particularly struck that IKZF1-expressing tumors responded significantly better to anti-PD-1 and anti-CTLA-4 treatment. Tumor growth was almost completely suppressed,” said study co-author Charles Drake, M.D., Ph.D., professor of medicine and director of genitourinary oncology at Columbia University Vagelos College of Physicians and Surgeons, co-director of the immunotherapy program, and associate director for clinical research of the Herbert Irving Comprehensive Cancer Center at CUIMC.
The predictions were first tested in a mouse model of melanoma in which the tumors were genetically modified to express IKZF1. The mice were found to have increased levels of infiltrating immune cells in their tumors, compared to control mice with conventional melanoma, a sign that the tumors had lost at least some ability to evade the immune response.
The team then analyzed data from a previous study of melanoma patients with disabled IKZF1. Patients with disabled IKZF1 had higher recurrence rates and worse survival compared to other melanoma patients. Now, the investigators are searching for additional candidate genes that can similarly be used to enhance the response to immunotherapy in melanoma.
The algorithm also predicted that prostate cancer could be made more responsive to immunotherapy. In lab experiments, the team found that restoring IKZF1 activity in prostate tumor cells made them susceptible to immunotherapies.
“Clinically, this is an especially exciting finding, since prostate cancer is generally very poorly infiltrated by immune cells,” concluded Dr. Drake. “Turning these 'cold' tumors 'hot' could be a key to therapeutic success.”