Currently, only 10% of the drugs that enter Phase I receive marketing approval from the U.S. Food and Drug Administration (FDA), with unmanageable toxicity accounting for approximately 30% of the clinical failures for investigational new drugs (INDs).1,2 Safety-based discontinuation of INDs is mainly associated with cardiotoxicity (which is also one of the most common reasons for the withdrawal of marketed drugs). The discontinuation and/or withdrawal of some of these drugs could have been predicted preclinically with more thorough and more advanced safety screening, including validated Good Laboratory Practice (GLP) in vitro screening assays.3
The most common in vivo screening assay is the QT interval measured from a surface electrocardiogram, which represents the summation of the action potentials of ventricular cardiomyocytes (Figure 1A). Prolongation of the rate-corrected QT interval beyond 440 ms is associated with an increased risk of the polymorphic ventricular tachycardia (increased heart rate) called torsades de points (TdP), which is characterized by a “twisting of the points” around the isoelectric line (Figure 1B). Although TdP is not itself fatal, it can lead to life-threatening ventricular fibrillation and sudden cardiac death.4,5

Mutations in 16 different genes have been linked to familial forms of long QT syndrome. However, certain drugs have a propensity to prolong the QT interval and are associated with an increased risk of TdP. Although the incidence of drug-induced QT prolongation and TdP is low, the mortality rate is between 10% and 20%.6
Between 1990 and 2006, drug-induced QT prolongation and TdP presented a significant safety challenge, resulting in the withdrawal of several drugs (for example, cisapride) from the market due to their proarrhythmic liability.7 It was later discovered that these drugs inhibited the human ether-à-go-go related gene (hERG) potassium channel. This ion channel controls the flow of potassium ions from within ventricular cardiomyocytes into the extracellular space. The channel activates rapidly upon initiation of the action potential (depolarization), which underlies why it is referred to as the rapid delayed rectifier potassium current (IKr). This current is essential for controlling the duration of ventricular action potentials and, therefore, fundamental to controlling the QT interval.
Responding to this challenge in 2005, the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH) released nonclinical and clinical cardiac risk evaluation guidelines (ICH E14/S7B). As part of the ICH guidelines, in vitro hERG screening during drug discovery and nonclinical drug development is now mandatory for screening small-molecule INDs to detect proarrhythmic activity.8
Additionally, a recent update to the guidelines allows for the use of validated GLP in vitro screening and in vivo QTc-negative results to waive the need for a clinical thorough QT (TQT) study.
In vitro GLP-compliant hERG screening
The introduction of in vitro ICH-mandatory GLP-compliant hERG screening during drug discovery and nonclinical drug development has significantly reduced the development of proarrhythmic drugs,9 and so far, it has successfully prevented any further new drug withdrawals from the market due to TdP causation.7
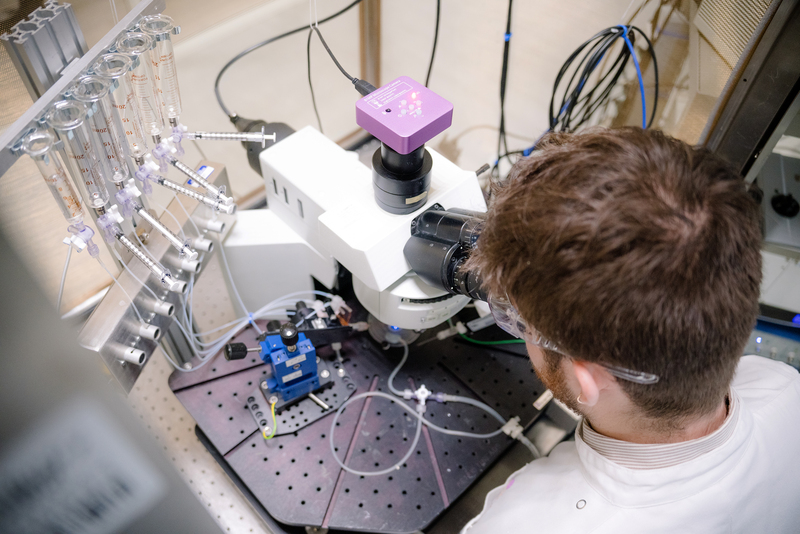
The GLP assessment of compounds against hERG is most commonly performed using the conventional whole-cell patch-clamp technique. For this assay, the hERG channel is overexpressed in a recombinant cell expression system, such as Chinese hamster ovary cells. The conventional whole-cell patch-clamp technique involves establishing a seal between the tip of a glass pipette electrode and the membrane of the cell expressing hERG. Once the seal has been obtained, negative pressure and/or electrical current is used to rupture the cell membrane and produce the whole-cell configuration.10 The glass pipette contains an electrode that is in contact with the intracellular solution of the cell. A ground electrode is located in the bath, which allows the voltage across the cell membrane to be clamped; this allows the operator to control the function of voltage-sensitive ion channels, such as hERG.
Once the whole-cell configuration has been achieved, the FDA’s recommended voltage protocol can be used to elicit hERG current. Initially, the cell is superfused with a vehicle control solution to generate a baseline reading (Figure 2A). Once the hERG current has stabilized, the cell can be superfused with a test solution to determine whether it inhibits the hERG current. Figure 2B shows the effect of 1 and 10 µM ondansetron (an antiemetic agent) on the hERG current. There was a rapid and concentration-dependent inhibition of hERG. A supramaximal concentration of a positive control compound, E-4031, was used to fully block hERG current at the end of each experiment. These assays support the preclinical stages of drug development. A conventional whole-cell patch-clamp technique measuring biological electrophysiology (ion currents) can be performed as a “gold standard” following the FDA’s recommended voltage protocols to study drug-cardiac ion channel interactions before first-in-human studies.9

Vital importance of high-quality data
The ICH S7B guidelines stipulate that in vitro hERG assessments should be performed to GLP compliance. In addition, the recently released ICH E14/S7B 2022 Q&A provides recommendations on the experimental methods that should be employed, the quality control parameters for analyzing the data, and the preferred format for reporting the data.9 In line with the best practice recommendations, Metrion Biosciences developed and validated its own GLP hERG assay.
Case study: GLP-compliant hERG assay validation
The study, conducted to GLP compliance, used the conventional whole-cell patch-clamp technique to establish potency data and safety margins for the FDA’s three recommended positive control drugs: ondansetron, moxifloxacin (antibiotic), and dofetilide (antiarrhythmic), which each have well-defined torsadogenic (TdP causing) risk profiles.11 The FDA’s QC parameters were monitored during the experiment and during offline analysis to ensure high data quality.
The relative potency of a drug to inhibit the hERG current is expressed as the half-maximal inhibition concentration (IC50), which is the drug concentration at which 50% of the hERG current is inhibited.12 The IC50 values and associated safety margins generated for the three compounds in the study were consistent (within a twofold difference) with the values published in the E14/S7B 2022 training materials (Figure 3). In addition, the IC50 value generated for ondansetron (1.55 µM 95% CI: 1.25 to 1.93) was consistent with that generated from a previous non-GLP study performed at the same test facility (1.72 µM 95% CI: 1.51 to 1.95), which demonstrates the consistency of this established assay.
The GLP hERG assay was successfully validated by Metrion Biosciences using ondansetron, moxifloxacin, and dofetilide to U.K. GLP compliance and according to the experimental recommendations outlined in the ICH E14/S7B Q&A guidance (Figure 3). The potency of each standard was in alignment with the ICH E14/S7B training material values. This validation ensures that each IND assessed generates high-quality data ready for incorporation into small-molecule IND applications.

Thorough QT waivers
The recently released ICH E14/S7B 2022 Q&As provide an opportunity to combine GLP-compliant hERG data with in vivo corrected QT (QTc) data into an integrated risk assessment pathway, which may negate the need to perform a clinical TQT study.
Compounds displaying a negative result for both the in vivo QTc and in vitro GLP-compliant hERG studies with respect to their respective safety margins over the expected free clinical exposure are considered to have a “double negative” profile. These data can be used to generate a TQT waiver application that may, if accepted by the regulatory authorities, negate the need to run a clinical TQT study.
Clinical TQT studies can be overly sensitive but not very specific, resulting in false positives where candidate compounds might not be proarrhythmic in nature.13 Furthermore, clinical TQT studies are costly, usually ranging between $2 million and $4 million. While this may represent less than 1% of the overall cost of taking a drug to market, it is still a major expense, especially given that each IND needs to be screened.14
Obtaining a waiver by achieving a “double negative” result can save time, reduce costs, and conserve resources significantly. For this, high-quality data for full candidate concentration-response curves and a suitable reference standard that matches the FDA’s data are critical. Expertise in this area is essential for expediting such testing and ensuring high-quality data generation and reporting.
Conclusion
It is of significant benefit to drug discovery scientists to identify potentially proarrhythmic drugs at the preclinical stage. The recently released ICH E14/S7B 2022 Q&As recognize the value of preclinically validated in vitro GLP-compliant hERG studies in predicting the liability of potentially proarrhythmic drugs. Importantly, when this assay is used with in vivo QTc data, it can waive the need for costly and time-consuming clinical TQTs—potentially accelerating the delivery of promising new candidate drugs to market and, critically, to patients in need.
Steve Jenkinson, PhD, is vice president of drug discovery and safety assessment at Metrion Biosciences.
References
1. Dowden H, Munro J. Trends in clinical success rates and therapeutic focus. Nat. Rev. Drug Discov. 2019 Jul; 18(7): 495–496. DOI: 10.1038/d41573-019-00074-z. PMID: 31267067.
2. Harrison RK. Phase II and phase III failures: 2013–2015. Nat. Rev. Drug. Discov. 2016 Dec; 15(12): 817–818. DOI: 10.1038/nrd.2016.184. Epub 2016 Nov 4. PMID: 27811931.
3. Laverty H, Benson C, Cartwright E, et al. How can we improve our understanding of cardiovascular safety liabilities to develop safer medicines? Br. J. Pharmacol. 2011 Jun; 163(4): 675–693. DOI: 10.1111/j.1476-5381.2011.01255.x. PMID: 21306581; PMCID: PMC3111672.
4. Mayo Foundation for Medical Education and Research. Long QT syndrome. Accessed Jan 18, 2024.
6. Li D, Chai S, Wang H, et al. Drug-induced QT prolongation and torsade de pointes: A real-world pharmacovigilance study using the FDA Adverse Event Reporting System database. Front. Pharmacol. 2023 Dec 21; 14: 1259611. DOI: 10.3389/fphar.2023.1259611. PMID: 38186652; PMCID: PMC10771307.
7. Krumpholz L, Wiśniowska B, Polak S. Correction to: Open-access database of literature derived drug-related Torsade de Pointes cases. BMC Pharmacol. Toxicol. 2022 Jan 31; 23(1): 11. DOI: 10.1186/s40360-022-00550-0. Erratum for: BMC Pharmacol. Toxicol. 2022 Jan 10; 23(1): 7. PMID: 35101142; PMCID: PMC8802418.
8. Qu Y, Kirby R, Davies R, et al. Time Is a Critical Factor When Evaluating Oligonucleotide Therapeutics in hERG Assays. Nucleic Acid Ther. 2023 Apr; 33(2): 132–140. DOI: 10.1089/nat.2022.0043. Epub 2022 Dec 26. PMID: 36576986; PMCID: PMC10066779.
9. GLP hERG Screening. 2023.
10. Zeng H, Kang J. In vitro Testing of Proarrhythmic Toxicity. In: Zhang D, Surapaneni S, eds. ADME-Enabling Technologies in Drug Design and Development. Hoboken, NJ: John Wiley & Sons; 2012.
11. Masterton J, Tokar S, Jinat A, Kirby R. (2024). GLP hERG Assay Validation following ICH E14/S7B 2022 Q&A best practice guidelines. Posted 2024 Feb 1. Accessed 2024 Apr 2.
12. Shah RR. The significance of QT interval in drug development. Br. J. Clin. Pharmacol. 2002 Aug; 54(2): 188–202. DOI: 10.1046/j.1365-2125.2002.01627.x. PMID: 12207642; PMCID: PMC1874403.
13. Turner JR, Karnad DR, Cabell CH, Kothari S. Recent developments in the science of proarrhythmic cardiac safety of new drugs. Eur. Heart J. Cardiovasc. Pharmacother. 2017 Apr 1; 3(2): 118–124. DOI: 10.1093/ehjcvp/pvw045. PMID: 28363206.
14. Callahan T. The Future of QT in Clinical Trials. App. Clin. Trials. 2014 Sept 22.