By Yuwen Wang and Andy Tay, PhD
Chimeric antigen receptor T (CAR-T) cell therapy has significantly transformed the management of cancer, specifically in patients suffering from leukemia and lymphoma. This treatment approach entails the isolation of T cells from the patient, genetic modification to introduce CARs on their surface, and reintroduction back into the patient’s bloodstream.1 Through CARs, T cells are enabled to identify and eliminate cancerous cells expressing the antigen of interest.
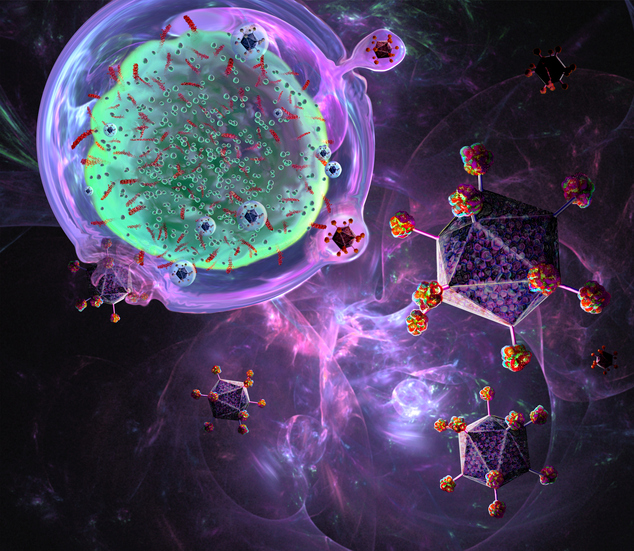
One of the key manufacturing steps for CAR-T cells is to activate and expand them. This is particularly important because the clinical dose of CAR-T therapy is approximately one million cells/kg of patient weight, and for many terminally ill patients, they have very low numbers of healthy cells suitable for manufacturing. To activate T cells, manufacturers have created artificial antigen presenting cells (aAPC) such as microbeads coated with antibodies targeting CD3+ T cells and CD28 co-stimulatory molecule.2
Microbeads are spherical particles with a diameter of a few micrometers (1–5 µm), typically made of polymers or magnetic materials, which can be coated with specific antibodies or ligands to target and activate T cells. When these microbeads are co-cultured with CAR-T cells, they provide a more efficient way of activating and expanding CAR-T cells as compared to the use of actual APC like dendritic cells which contributes to manufacturing complexity.
When CAR-T cell therapies first started, microbeads were only coated with a single antibody targeting CD3 to bind to T cells. However, in the next generation of CAR-T manufacturing, multi-epitope microbeads that display multiple antigens or epitopes were found to provide better CAR-T cell activation for expansion. An example of a multi-epitope microbead is the CD3/28 microbead, which is being used in CAR-T therapies to activate T cells and enhance their anti-tumor activity.

The predominant microbead used for clinical CAR-T manufacturing is DynabeadTM , which is made up of magnetic iron-oxide material that facilitates magnetic removal post-manufacturing which is key for regulatory approval.3 Its diameter is about 3 µm which minimizes endocytosis by CAR-T cells. Nevertheless, as Dynabeads are made of inorganic material, and it cannot be degraded by the cells during manufacturing. Hence, manufacturers have to invest in costly analytical tools to prove that >95% of Dynabeads are removed (as required by the FDA) which can increase the price of a CAR-T therapy.
Additionally, with increasing knowledge that the degree of TCR activation is influenced by the strength of mechanical binding between TCR and Dynabeads, there has been rising interest to explore ways to modify microbead designs such as stiffness and shape to improve CAR-T cell activation.
Biodegradable microbeads
Biodegradable microbeads have been developed to further enhance the activation of CAR-T cells. These microbeads are made of materials that degrade over time and can encapsulate nucleic acids, peptides, or small molecule drugs or act directly as immunostimulants as the material breaks down into lower molecular weight free polymers to enhance the efficacy of CAR-T cells.
One of the challenges of using traditional microbeads in CAR-T manufacturing as mentioned before is that they may not be completely removed after manufacturing and may persist in the body when CAR-T therapy is administered, potentially causing adverse effects such as inflammation. Biodegradable microbeads, on the other hand, are designed to break down over time and be safely eliminated by the body.
A team led by Jonathan Schneck, MD, PhD, professor of pathology, and Jordan J. Green, PhD, professor, biomedical engineering at the Johns Hopkins University, School of Medicine, developed a novel biodegradable microbead by combining poly(lactic acid-ethanolic acid copolymer) (PLGA) and cationic poly(β-amino-ester) (PBAE).4 The PLGA/PBAE aAPC demonstrated improved surface interactions with antigen specific CD8+ T cells and resulted in enhanced T cell activation and expansion in vitro, which was positively associated with a significant increase in the efficiency of T-cell stimulation signals.
Importantly, the PLGA/PBAE aAPC can also amplify cytotoxic CD8+ T cells specific to the antigen in vivo. In an experimental mouse model with B16-F10 melanoma, the combination of PLGA/PBAE aAPC with checkpoint therapy resulted in decreased tumor growth and longer survival rates. These findings highlight the potential of PLGA/PBAE aAPC as a compatible microbead for T-cell activation.
Shape-variable microbeads
The morphology of aAPC, in addition to the material used, can be a crucial factor in achieving optimal aAPC-T cell interaction and subsequent T cell activation. A group of researchers led by Jan van Hest, PhD, professor and Loai Abdelmohsen, PhD, assistant professor, both from Eindhoven University of Technology, created polymer vesicles using poly(ethylene glycol)-block-poly(d,l-propanediol) (PEG-PDLLA).5
By modifying the presence of organic solvents during the self-assembly process, they were able to influence the flexibility of the polymers and control both their sizes and shapes. This approach resulted in the transformation of spherical polymers into tubular variants through extrusion and permeation, allowing for greater control over aAPC morphology.
Their results show that high ligand densities are crucial for enhanced T-cell activation, which can be further improved by using larger size polymer vesicles. Additionally, the shape and size of the polymer vesicles play an important role in the activation of T cells. The results indicate that large, elongated polymer vesicles are more effective in activating T cells than spherical (existing designs used clinically) or smaller polymer vesicles, particularly at low ligand densities.
“Our main motivation is that until now a systematic study of the effect of nanoparticle topology on T-cell activation was missing. With our system we could keep the chemical composition of all our particles identical while varying size, shape, and antibody density in a controlled fashion. Based on these findings we are now working towards in vivo applications of our platform,” says van Hest.
These findings demonstrate the potential of shape-variable polymer vesicles as aAPCs and emphasize the importance of topology in their rational design. Another likely reason is that anisotropic particles with non-spherical shapes are less likely to be taken up by cells. The ability to manipulate the size and shape of the polymer vesicles and their ligand density holds great promise for the development of more efficient aAPCs for T cell activation.
Microbeads in biomaterial scaffolds
In addition to epitopes, materials, and shapes, another promising direction is to incorporate microbeads into biomaterial scaffolds to enhance CAR-T cell efficacy. Scaffolds provide a three-dimensional structure that mimics the natural environment of T cells, and microbeads can further enhance T-cell activation and improve overall CAR-T cell therapy efficacy.
A team led by David Mooney, PhD, professor, Harvard University, developed a new system to generate T cells using scaffolds that mimic the activation of T cells by APCs in vivo.6,7 This scaffold is composed of biodegradable microrods loaded with interleukin 2 and coated with a supporting lipid bilayer. The lipid membrane can be customized with various T cell activating molecules to selectively expand T cells with greater efficiency and control than standard methods.

Human T-cell populations show significant expansion after a single dose of stimulation with the APC mimetic scaffold (APC-ms), surpassing current standard methods without compromising functionality. In a mouse model using CAR-T cells to target lymphomas, the scaffold enabled greater T-cell expansion and robust efficacy compared to current standards.
Personalizing CAR-T cell stimulation during the manufacturing process has been shown to significantly enhance the consistency and effectiveness of the resulting CAR-T cell products. Researchers have also utilized artificial APC-ms to fine-tune T cell stimulation levels to modulate T-cell phenotype obtained from leukemia patients, leading to a significant improvement in tumor clearance in vitro and in vivo. This novel system holds great promise for the development of next-generation CAR-T cell immunotherapies that can be personalized to address individual patient requirements.
“CAR-T cell responses can be variable and inconsistent, and this can result in poor patient outcomes. This is likely due at least in part to the varying health of the patients from whom the therapy is manufactured. We hope that our work allows for a more flexible manufacturing approach that allows personalization of the manufacturing of CAR-T products, resulting in highly therapeutic products for all patients,” says Mooney.
In contrast to microbeads, nanoparticles or nanobeads are also considered by researchers as potential candidates for activation of T cells as aAPCs.8 Ben-Akiva and colleagues synthesized biodegradable anisotropic ellipsoidal-shaped aAPC nanoparticles to improve CAR-T cell activation better than spherical-shaped aAPC nanoparticles. The former also had improved pharmacokinetic properties to activate CAR-T cells in vivo for cancer treatment.
However, one limitation of using nanoparticles as aAPCs is their size. Nanoparticles are much smaller than cells compared to microbeads and are more likely to be endocytosed, causing cytotoxicity. Nanoparticles might also have limited surface areas to have high enough ligand density to activate T cells. Importantly, as nanoparticles are smaller, when they are made of inorganic material, manufacturers would have more difficulty proving that they are removed as compared to larger microbeads.
Outlook
The field of CAR-T cell therapy has rapidly progressed over the past decade, and to make this promising treatment more accessible, CAR-T manufacturing needs to be more robust. Currently, 3 µm iron-oxide microbeads coated with antibodies targeting CD3 and CD28 are still the only clinical product used. This is despite studies showing that polymeric materials that offer biodegradability and programmable size, shape and ligand density may be advantageous at the preclinical level.
In addition, there is also rising interest in the use of biomaterial scaffolds loaded with microbeads to boost CAR-T manufacturing in vitro and in vivo. These innovations are expected to bring CAR-T therapy to the patients who need it the most.
Andy Tay, PhD, is a professor at the National University of Singapore and a freelance writer. Yuwen Wang is a PhD student at the university.
References
- Feins, S., Kong, W., Williams, E. F., Milone, M. C., & Fraietta, J. A. (2019). An introduction to chimeric antigen receptor (CAR) T-cell immunotherapy for human cancer. American Journal of Hematology, 94(S1), S3–S9.
- Neal, L. R., Bailey, S. R., Wyatt, M. M., Bowers, J. S., Majchrzak, K., Nelson, M. H., Haupt, C., Paulos, C. M., & Varela, J. C. (2017). The Basics of Artificial Antigen Presenting Cells in T Cell-Based Cancer Immunotherapies. Journal of Immunology Research and Therapy, 2(1), 68–79.
- Stock, S., Schmitt, M., & Sellner, L. (2019). Optimizing Manufacturing Protocols of Chimeric Antigen Receptor T Cells for Improved Anticancer Immunotherapy. International Journal of Molecular Sciences, 20(24).
- Rhodes, K. R., Isser, A., Hickey, J. W., Ben-Akiva, E., Meyer, R. A., Kosmides, A. K., Livingston, N. K., Tzeng, S. Y., Schneck, J. P., & Green, J. J. (2021). Biodegradable Cationic Polymer Blends for Fabrication of Enhanced Artificial Antigen Presenting Cells to Treat Melanoma. ACS Applied Materials & Interfaces, 13(7), 7913–7923.
- Wauters, A. C., Scheerstra, J. F., Vermeijlen, I. G., Hammink, R., Schluck, M., Woythe, L., Wu, H., Albertazzi, L., Figdor, C. G., Tel, J., Abdelmohsen, L. K. E. A., & van Hest, J. C. M. (2022). Artificial Antigen-Presenting Cell Topology Dictates T Cell Activation. ACS Nano, 16(9), 15072–15085.
- Cheung, A. S., Zhang, D. K. Y., Koshy, S. T., & Mooney, D. J. (2018). Scaffolds that mimic antigen-presenting cells enable ex vivo expansion of primary T cells. Nature Biotechnology, 36(2), 160–169.
- Zhang, D. K. Y., Adu-Berchie, K., Iyer, S., Liu, Y., Cieri, N., Brockman, J. M., Neuberg, D., Wu, C. J., & Mooney, D. J. (2023). Enhancing CAR-T cell functionality in a patient-specific manner. Nature Communications, 14(1), 506.
- Ben-Akiva, E., Hickey, J. W., Meyer, R. A., Isser, A., Shannon, S. R., Livingston, N. K., Rhodes, K. R., Kosmides, A. K., Warren, T. R., Tzeng, S. Y., Schneck, J. P., & Green, J. J. (2023). Shape matters: Biodegradable anisotropic nanoparticle artificial antigen presenting cells for cancer immunotherapy. Acta Biomaterialia, 160, 187–197.