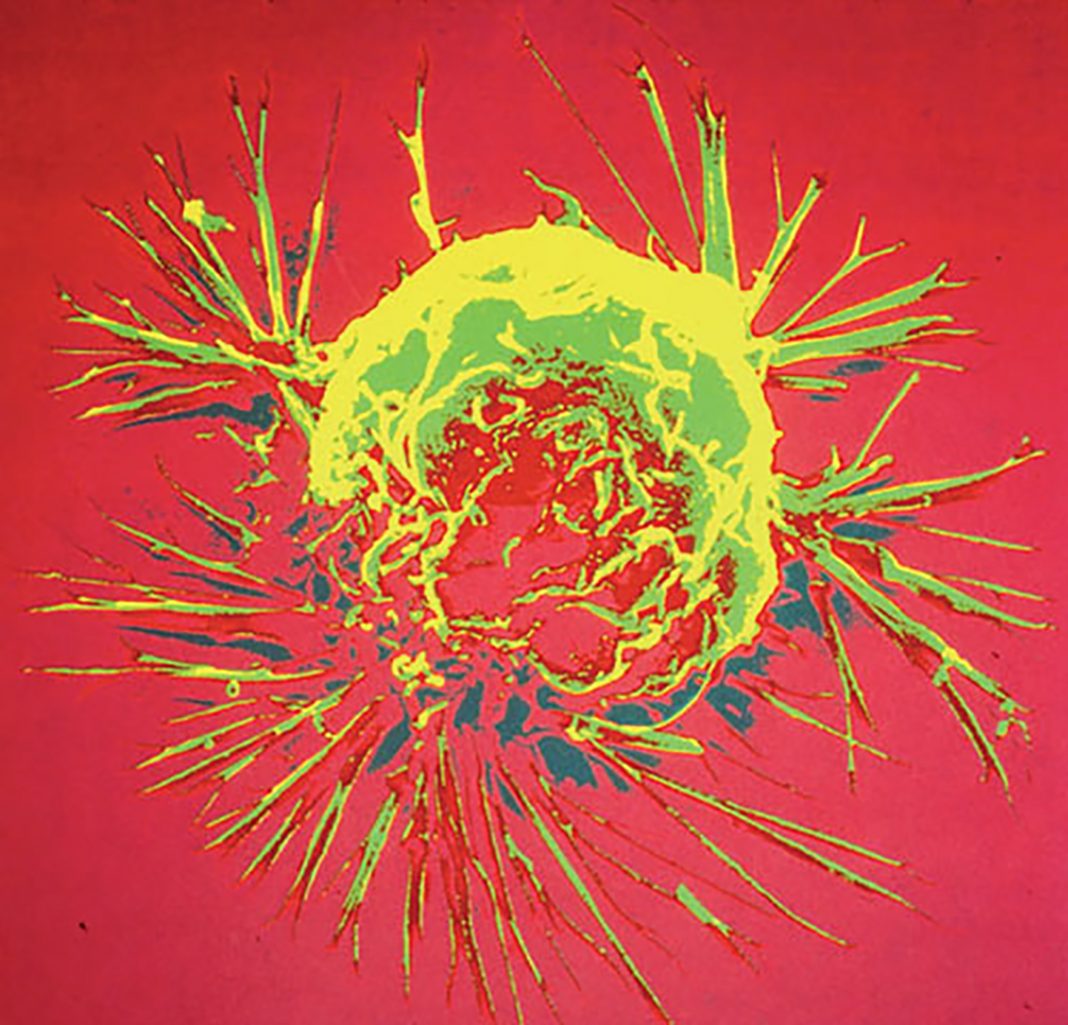
A drug previously approved for treating migraine and epilepsy has been found to slow the growth of triple negative breast cancer in mouse models. Researchers in the U.S., Taiwan, and China carried out screening studies to identify known pharmacologically active compounds that trigger degradation of N-Ras, a key protein that drives the development of aggressive basal-like breast cancer (BLBC). The assays highlighted flunarizine (FLN) as a promising candidate, and subsequent in vitro studies confirmed that the drug selectively blocked the growth of BLBC cells, but not other subtypes of breast cancer cells, and also inhibited tumor growth in an in vivo BLBC xenograft model.
“We focused on finding ways to disrupt the effects of a class of protein called Ras, which are powerful drivers of a wide range of cancers,” comments Eric C. Chang, Ph.D., associate professor of molecular and cellular biology at the Lester and Sue Smith Breast Center in the Dan L. Duncan Comprehensive Cancer Center at Baylor College of Medicine. “In this proof-of-concept study, we have established a strategy to target N-Ras for therapy.”
The Baylor College of Medicine team, headed by Ze-Yi Zheng, Ph.D., together with colleagues at the Houston Methodist Research Institute, the Hospital (TCM) Affiliated to Southwest Medical University (China), and the National Taiwan University Hospital and National Taiwan University College of Medicine (Taiwan), report on their work in a paper published today in Scientific Reports, which is titled, “Induction of N-Ras degradation by flunarizine-mediated autophagy.”
Humans have three RAS genes, H-, N-, and K-Ras, the authors explain. More than 30% of all human tumors contain oncogenic RAS mutations, and while K-Ras is the most frequently mutated RAS gene in cancers generally, N-Ras mutations also occur in certain cancer types. Yet despite the importance of Ras in cancer, there are no drugs that specifically target the Ras proteins. Current approaches are designed to reduce membrane affinity for Ras proteins, block Ras-effector interaction, or inhibit the activity of effector protein kinases such as B-Raf, the authors continue. However, tumors commonly develop resistance through mechanisms that thwart the continued effectiveness of these therapeutic approaches. “Therefore it seems highly desirable to target Ras proteins themselves in order to shut down all of their oncogenic potential at the root,” the team writes.
One potential therapeutic avenue is to control Ras post-transcriptionally by proteolysis. The researchers devised a screening strategy that aimed to identify and repurpose already FDA-approved drugs that can also induce Ras degradation. “Our assay allows us to visually determine which drugs promote N-Ras degradation,” Dr. Chang explains. “We tagged N-Ras proteins with a green fluorescent tag. If the fluorescent N-Ras proteins were destroyed, the fluorescence would be lost.”
The assay identified the calcium ion channel blocker flunarazine, which is commonly used to treat conditions including epilepsy. “Flunarizine has been used in medical practice for decades to treat dizziness and vertigo and to prevent migraines,” Dr. Chang comments. Interestingly, while flunarazine hasn’t previously been used to treat cancer, prior research has shown that it can boost the sensitivity of cancer cells to some chemotherapy agents.
The team’s subsequent studies indicated that flunarazine induced N-Ras degradation by autophagy, and in vitro tests showed that the drug inhibited the growth of BLBC cells specifically. This growth inhibition could be further enhanced by combining flunarazine with drugs that target other components of the N-Ras pathway.
In a final round of experiments the researchers demonstrated that flunarazine therapy reduced the growth of human BLBC tumors in mice. “Our data showed that when FLN was added at levels comparable to those used in humans, tumor growth was efficiently inhibited, mimicking the effect of doxycycline (DOX)-inducible N-Ras silencing,” they comment.
The authors acknowledge that further studies will be needed to define why and how flunarazine therapy leads to N-Ras degradation in BLBC cells. Nevertheless, they write, “ … this proof-of-principle study presents evidence that the autophagy pathway can be coerced by small molecule inhibitors, such as FLN, to degrade Ras as a strategy to treat cancer. FLN has low toxicity and should be further investigated to enrich the toolbox of cancer therapeutics.”
They also note that the studies validate the use of their screening approach to identify and repurpose existing drug compounds against cancer. “Screening existing relatively safe drugs for new functions is a valuable strategy for identifying drugs that can potentially be used to treat diseases for which currently there are no available treatments,” Dr. Chang states. “Reprogramming pathways that degrade cellular materials may be an effective strategy to remove a cancer driver that is otherwise hard to target.”