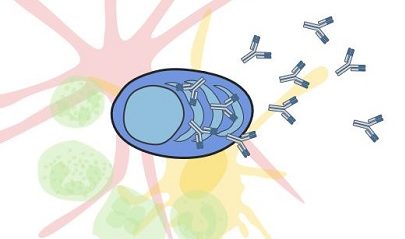
The longer plasma cells live, the longer they secrete the antibodies that protect us from infection. Some plasma cells persist for decades, whereas others disappear after just a few months. To uncover the secrets of long-lived plasma cells (LLPCs), researchers at Monash University led by Marcus J. Robinson, PhD, and David M. Tarlinton, PhD, studied how they accumulate in one of their favorite survival niches, the bone marrow. The researchers hoped that by “tracking the pathway to immunity,” they could learn how vaccines could be formulated and administered to enhance antibody-mediated protective immunity.
The researchers employed a technique called genetic timestamping to track the generation and recruitment of LLPCs to bone marrow in mice vaccinated with a model antigen. At various time points in the three months following vaccination, the researchers gave the mice a drug called tamoxifen, which caused expression of reporter genes, thereby marking only the subset of LLPCs that became activated within a few days of drug injection.
The results of this work appeared in Science Immunology, in an article titled, “Long-lived plasma cells accumulate in the bone marrow at a constant rate from early in an immune response.”
“[We] show that persistent PCs accrue in bone marrow at an approximately constant rate of one cell per hour over a period spanning several weeks after a single immunization with a model antigen,” the article’s authors wrote. “Affinity-based selection was evident in persisting PCs, reflecting a relative and dynamic rather than absolute affinity threshold as evidenced by the changing pattern of VH gene somatic mutations conveying increased affinity for antigen.”
According to Tarlinton, studying individual plasma cells as they are born, mature, enter storage, and persist (or not) “can inform our understanding of how the recruitment of long-lived plasma cells occurs.” Tarlinton and colleagues noted that “possible mechanisms for recruiting new specificities while maintaining homeostasis are that nascent PCs actively displace existing LLPCs or that nascent PCs occupy a vacant niche.” That is, the mechanism in operation may involve displacement or replenishment. The view favored by Tarlinton and colleagues is that “newly generated PCs occupy survival niches made vacant by intrinsic turnover within the existing LLPC population.”
By tracking plasma cells, the researchers found that one particular vaccination in a mouse led to the generation of around 40,000 persisting plasma cells in the bone marrow. These cells, after the initial flourish, then declined at a rate of around 0.1% a day with a half-life of about 700 days, providing both an estimate of the duration of protection and identifying for further study the long-lived cells themselves.
Tarlinton stresses that understanding how LLPCs are generated, live, and die “will inform our ability to modulate their recruitment, through different vaccine combinations or delivery strategies—ultimately allowing us to be able to increase the longevity of immunity.”
“Understanding LLPC formation will inform our ability to modulate their recruitment, whether this be via the mechanics of differentiation in the germinal center or the means by which LLPCs interact with niches,” the authors of the current study concluded. “If LLPCs are recruited at a constant rate, then extending the duration of the germinal center reaction by tuning inputs, for example, through different adjuvant combinations or antigen delivery strategies, could extend PC differentiation and thus increase long-term antibody titers.”
In a recent review article, Tarlinton and colleagues suggested that competition between plasma cells for survival cues occurs, such that there could be a “survival of the fittest” bent to long-term antibody-based immunity. (This article appeared in Immunological Reviews and was titled, “How intrinsic and extrinsic regulators of plasma cell survival might intersect for durable humoral immunity.”)