![Drug-resistant <i>Streptococcus pneumoniae</i>. [CDC]” /><br />
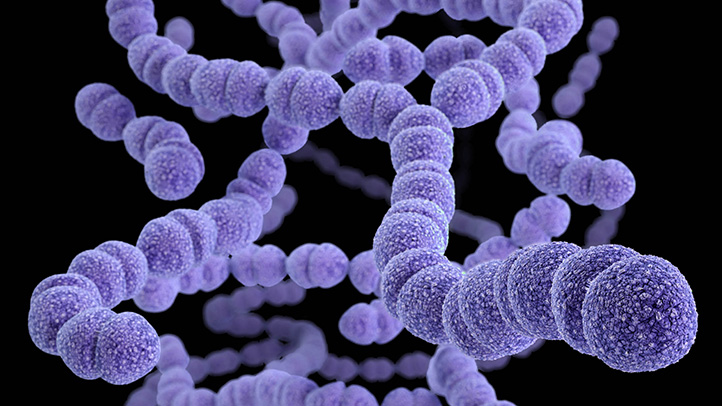
<span class=](https://genengnews.com/wp-content/uploads/2018/08/drugresistantbacteria06722x4061892181482-1.jpg) Drug-resistant Streptococcus pneumoniae. [CDC]
Drug-resistant Streptococcus pneumoniae. [CDC]
Any assistance in the fight to thwart efforts of microbial pathogens to sidestep antibiotic drug mechanisms is a welcome addition to the arsenal researchers and physicians use to treat bacterial infections. Now, a team of investigators led by scientists at Oregon State University (OSU) has developed a new molecule that neutralizes a microbe’s ability to destroy antibiotic compounds.
Beta-lactamases (also known as penicillinase) are a family of enzymes that are genetically encoded by many bacteria and destroy a wide range of antibiotic drugs, such as penicillins, cephamycins, and even some carbapenems, which are often the last line defense against certain microbial infections. This family of enzymes is responsible for conferring multidrug resistance in many bacterial species.
The new molecule—named PPMO, short for peptide-conjugated phosphorodiamidate morpholino oligomer—was able to inhibit expression of a beta-lactamase molecule known as NDM-1, or New Delhi metallo-beta-lactamase.
“We're targeting a resistance mechanism that's shared by a whole bunch of pathogens,” explained co-lead study investigator Bruce Geller, Ph.D., professor of microbiology in OSU's College of Science and College of Agricultural Sciences. “It's the same gene in different types of bacteria, so you only have to have one PPMO that's effective for all of them, which is different than other PPMOs that are genus specific.”
The researchers were able to demonstrate in vitro that PPMO restored the ability of an antibiotic—in this case, meropenem, an ultra-broad-spectrum drug of the carbapenem class—to fight three different genera of bacteria that express NDM-1. The OSU team also showed that a combination of PPMO and meropenem was effective in treating mice infected with a pathogenic strain of Escherichia coli that is NDM-1 positive.
The findings from this study were published recently in the Journal of Antimicrobial Chemotherapy in an article entitled “Peptide-Conjugated Phosphorodiamidate Morpholino Oligomer (PPMO) Restores Carbapenem Susceptibility to NDM-1-Positive Pathogens In Vitro and In Vivo.”
“We've lost the ability to use many of our mainstream antibiotics,” Dr. Geller noted. “Everything's resistant to them now. That's left us to try to develop new drugs to stay one step ahead of the bacteria, but the more we look, the more we don't find anything new. So, that's left us with making modifications to existing antibiotics, but as soon as you make a chemical change, the bugs mutate, and now they're resistant to the new, chemically modified antibiotic.”
That progression, De. Geller explained, made the carbapenems our last line of defense against bacterial infection. Yet, the researchers are optimistic about their results and noted that PPMO would likely be ready for testing in humans in about three years.
“The significance of NDM-1 is that it is destroys carbapenems, so doctors have had to pull out an antibiotic, colistin, that hadn't been used for decades because it's toxic to the kidneys,” Dr. Geller remarked. “That is literally the last antibiotic that can be used on an NDM-1-expressing organism, and we now have bacteria that are completely resistant to all known antibiotics. But a PPMO can restore susceptibility to antibiotics that have already been approved, so we can get a PPMO approved and then go back and use these antibiotics that had become useless.”