Researchers at Washington State University (WSU) have developed a novel, patent-pending treatment for diseases associated with inflammatory responses, including sepsis, stroke, rheumatoid arthritis, acute lung injury, and atherosclerosis. The new approach, described in Science Advances (“Nanoparticle-induced neutrophil apoptosis increases survival in sepsis and alleviates neurological damage in stroke“), uses protein nanoparticles (NPs) to deliver the cell-killing drug doxorubicin (DOX) directly to the activated neutrophils that drive the exaggerated immune response involved in inflammatory diseases. Laboratory studies and tests in live mice showed that treatment using the nanoparticles specifically killed activated neutrophils without compromising the immune system, led to increased survival in a mouse model of sepsis, and prevented brain damage in a mouse model of stroke.
“Scientists have started realizing that neutrophils—which were always seen as the ‘good guys’ for the key role they play in our immune system—are actually also contributing to the pathology of all kinds of diseases,” said the study’s senior author Zhenjia Wang, PhD, an associate professor in the WSU College of Pharmacy and Pharmaceutical Sciences. “Our experiment found that our doxorubicin albumin nanoparticles can decrease the lifespan of harmful neutrophils in the bloodstream. More importantly, we also found that our nanoparticles don’t inhibit the neutrophils’ function in the bone marrow.”
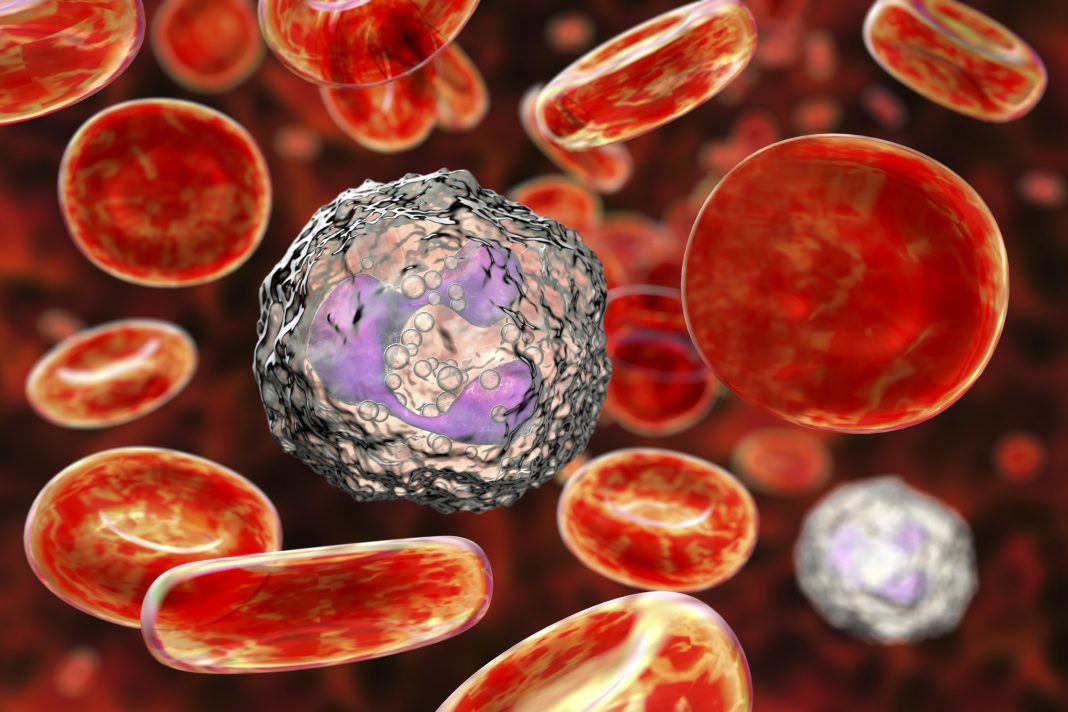
Polymorphonuclear neutrophils (PMNs) make up 50–70% of the white blood cells in humans, and these cells play a key role in the innate immune response to infections or tissue injury, the authors explained. Produced in the bone marrow, neutrophils effectively represent the immune system’s first line of defense, circulating in the blood and fending off invading viruses, bacteria, and other pathogens.
Neutrophils are short-lived cells, with a circulating lifespan of just 8–20 hours, after which they return to the bone marrow to die by apoptosis, a form of programmed cell death that helps to keep the numbers of neutrophils in balance. “Apoptosis is a natural process of cell death to maintain body homeostasis,” the investigators noted. “For example, neutrophils have a short life span, and it is regulated by apoptosis to preserve constant numbers of neutrophils in circulation to warrant immune homeostasis, protecting the host damage from neutrophils.”

Inflammation caused by pathogens or damaged tissue activates the circulating neutrophils and effectively extends their lifespan. This increases neutrophil numbers in the blood and can allow them to invade and accumulate in healthy tissue, resulting in damage to organs and potentially death. “…dysregulation of neutrophil trafficking may cause inflammatory and autoimmune disorders,” the researchers commented. “Neutrophils don’t know who the enemies are,” Wang said. “They just attack, releasing all kinds of harmful proteins in the bloodstream. They will kill bacteria, but they will also kill healthy tissue in the body at the same time.”
Previous approaches designed to target these activated, inflammatory neutrophils have been flawed in that they also kill resting neutrophils in the bone marrow. This compromises the immune system and increases the chance of life-threatening, secondary infections. The researchers reasoned that a safer approach may be to somehow trigger apoptosis in just the inflammatory neutrophils. To do this they developed a strategy based on the combined use of nanoparticles and a common chemotherapy drug, doxorubicin, which kills cells by inducing cell death.“ … specifically targeting inflammatory neutrophils to promote their apoptosis in time may be a strategy for improved therapies of inflammatory diseases,” the authors suggested. “Inspired by this natural neutrophil apoptosis, we proposed a means to specifically target inflammatory neutrophils using NPs that deliver DOX to promote neutrophil apoptosis to treat inflammatory disorders.”
For their targeted approach, Wang and his research team created albumin nanoparticles that carry doxorubicin directly into inflammatory neutrophils. The nanoparticles target Fc-gamma receptors, which are present on all neutrophils, but which the researchers discovered are only activated in inflammatory neutrophils, not in resting neutrophils. This means the nanoparticles only bind and deliver cell-killing doxorubicin to the inflammatory neutrophils.
To ensure that the doxorubicin is only released once inside the inflammatory neutrophils, the doxorubicin is bound to the nanoparticles via a pH-sensitive linker. The drug remains bound to the nanoparticle in the slightly alkaline environment of the bloodstream, but once the nanoparticles bind to and are internalized into the activated neutrophils, the acidic cell interior triggers the nanoparticle-doxorubicin connection to cleave, releasing the drug into the cell.

Having tested the properties of the nanoparticles in lab-grown cells, the team then carried out a series of in vivo experiments. One set of tests evaluated the nanoparticles, termed DOX-hyd-BSA NPs, in a mouse model of sepsis, a life-threatening condition that results from widespread inflammation in the body, and which is the cause of more than a third of all hospital deaths. A second set of tests evaluated the nanoparticles in a mouse model of ischemic stroke, which is caused by a blood clot that obstructs blood and oxygen flow to the brain and triggers a harmful inflammatory response when blood flow is restored. The studies showed that treatment using the nanoparticles increased survival in sepsis and minimized neurological damage from stroke.
“In the LPS-induced sepsis mouse model, administration of DOX-hyd-BSA NPs increased mouse survival to 70 versus 10 to 20% for controls,” the team reported. “Further studies show that neutrophil apoptosis decreased neutrophil numbers in circulation and in the lungs, thus inhibiting neutrophil trafficking to mitigate systemic inflammation. We discovered that administration of DOX-hyd-BSA NPs did not impair neutrophil production in the bone marrow when we compared neutrophil counts in healthy mice … In the ischemic stroke mouse model, we have shown that inhibition of neutrophil trafficking by DOX-hyd-BSANPs rescued mouse neurological damage during reperfusion therapy to ischemic stroke.” And encouragingly, while high doses of doxorubicin in chemotherapy can damage the heart and cause systemic inflammation, the low doses used in the mouse studies didn’t show damaging effects.
The researchers say their results demonstrate a new concept for treating inflammatory diseases by specifically targeting the delivery of therapeutics to proinflammatory neutrophils. “Collectively, our studies reveal a new concept to develop anti-inflammatory therapies by targeting immune cell apoptosis pathways using NPs,” they concluded. “This new approach avoids the systemic suppression caused by currently used anti-inflammatory agents.” The researchers are hopeful that the strategy of targeting neutrophil apoptosis pathways using nanoparticles could have wide-ranging applications in inflammatory and autoimmune diseases.
Wang and his team plan to conduct additional research to gain even deeper insights into how their technology works on a molecular basis, and to further optimize it. The next step would be to test the technology in human clinical trials before it could be developed into a commercially available treatment strategy that could benefit patients.