Brown adipose tissue (BAT) dissipates energy as heat. In doing so, brown fat serves as a biological heater in humans—keeping newborns warm, and in adults, brown fat activation positively correlates with cardio-metabolic health. Although it is understood that BAT is lost during both obesity and aging, not much is known about BAT apoptosis.
Now, a team of researchers applied untargeted metabolomics to demonstrate that apoptotic brown adipocytes release a specific pattern of metabolites, enriched in purine metabolites. More specifically, the purine inosine was found to stimulate energy expenditure in brown adipocytes via cAMP/protein kinase A—a signaling function that regulates thermogenic fat and counteracts obesity.
This work is published in Nature, in the article, “Apoptotic brown adipocytes enhance energy expenditure via extracellular inosine.”
Nowadays, “we’re toasty warm even in winter,” explains Alexander Pfeifer, PhD, from the Institute of Pharmacology and Toxicology at the University of Bonn. “So, our body’s own furnaces are hardly needed anymore.” At the same time, people are eating an increasingly energy-dense diet and are also moving far less than our ancestors.
These factors are poison for brown fat cells: the cells gradually cease to function and eventually die. “Research groups around the world are therefore looking for substances that stimulate brown fat and thus increase fat burning,” says Pfeifer.
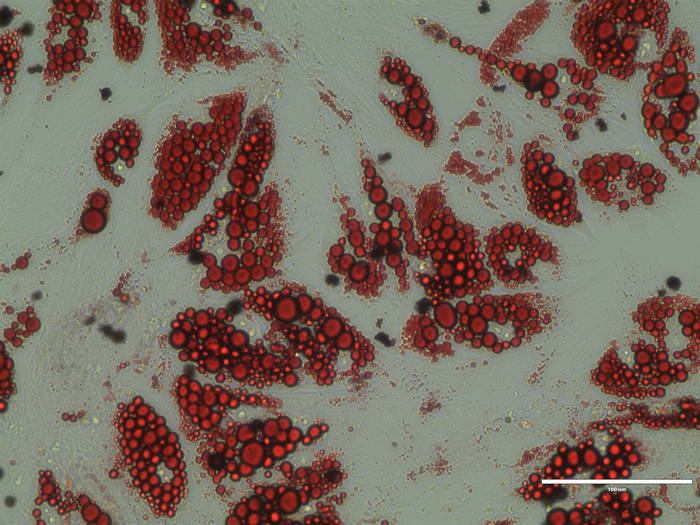
The team studied brown fat cells subjected to severe stress. “We found that they secrete the purine inosine in large quantities,” notes Birte Niemann, PhD, a researcher in the Pfeifer lab. In addition, intact brown fat cells were activated by inosine or by nearby dying cells.
Treatment of mice with inosine increased BAT-dependent energy expenditure and induced “browning” of white adipose tissue. In addition, mice fed a high-energy diet and treated with inosine at the same time remained leaner compared to control animals and were protected from diabetes.
The team uncovered the mechanism behind this effect. The nucleoside transporter 1 (ENT1) regulates inosine levels in BAT. The authors write that, “ENT1-deficiency increases extracellular inosine levels and consequently enhances thermogenic adipocyte differentiation.”
“There is a drug that was actually developed for coagulation disorders, but also inhibits the inosine transporter,” says Pfeifer. “We gave this drug to mice, and as a result they burned more energy.”
More specifically, the pharmacological inhibition of ENT1 enhanced BAT activity and counteracted diet-induced obesity, respectively. In human brown adipocytes, the authors note, knockdown or blockade of ENT1 increased extracellular inosine, which enhanced thermogenic capacity.
Humans also have an inosine transporter. In two to four percent of all people, it is less active due to a genetic variation. “Our colleagues at the University of Leipzig have genetically analyzed 900 individuals,” Pfeifer explains. “Those subjects with the less active transporter were significantly leaner on average.”
These results suggest that inosine also regulates thermogenesis in human brown fat cells. Substances that interfere with the activity of the transporter could therefore potentially be suitable for the treatment of obesity. The drug already approved for coagulation disorders could serve as a starting point. “However, further studies in humans are needed to clarify the pharmacological potential of this mechanism,” Pfeifer says. He does believe that a pill alone will be the solution to the world’s rampant obesity pandemic. “But the available therapies are not effective enough at the moment,” he stresses. “We therefore desperately need medications to normalize energy balance in obese patients.”