Researchers at Columbia University Department of Biomedical Engineering have engineered a novel probiotic strain of bacteria that can safely deliver immune checkpoint inhibiting nanobodies directly to tumors. When tested in cancer-bearing mice, a single dose of the bacteria continuously produced and released the anti-PD-L1 and anti-CTLA-4 nanobodies, triggering an immune response that led to tumor regression. The researchers say the versatile probiotic platform could be used to deliver multiple immunotherapies simultaneously, enabling the release of effective therapeutic combinations within the tumor for hard-to-treat cancers.
“We wanted to engineer a safe probiotic vehicle capable of delivering immune checkpoint therapies locally to minimize side effects,” commented research lead Tal Danino, PhD, assistant professor of biomedical engineering, who is also a member of the Herbert Irving Comprehensive Cancer Center and Data Science Institute. “We also wanted to broaden the versatility of the system by producing a range of immunotherapeutic combinations, including cytokines that could further elicit antitumor immunity, but are otherwise difficult to systemically deliver because of toxicity concerns.”
Danino and colleagues at Columbia, and at the University of Washington, report on their developments in Science Translational Medicine, in a paper titled, “Engineered probiotics for local tumor delivery of checkpoint blockade nanobodies.”
Antibodies that target immune checkpoints, PD-L1 and CTLA-4 have “revolutionized the paradigm of cancer immunotherapy treatments,” achieving success in a subset of cancers, the authors wrote. However, systemic delivery of the antibodies can also cause substantial side effects, with up to 70% of patients reporting adverse reactions, ranging from skin rash and endocrine disorders to liver toxicity. And while combining checkpoint blockade therapies can further improve effectiveness, combining such drugs also leads to even more severe toxicity that can results in drug discontinuation. “Thus, there is a clear need for the improved delivery of immune checkpoint inhibitors to circumvent these limitations and to provide a more localized, sustained, and minimally invasive therapeutic option,” the team noted.
Advances in genetic technologies have allowed scientists to engineer “intelligent microbial delivery systems” that can be used to deliver therapeutics. Using synthetic biology its now possible to generate gene circuits that control bacterial growth and gene expression, and allow the microorganisms to sense and respond to conditions such as inflammation, infection and cancer. Bacteria will also preferentially accumulate in tumors, the team noted. “Because bacteria are both inherently present and selectively grow within tumors, they provide a natural platform for the development of programmable therapeutic delivery vehicles. … A multitude of studies has shown that systemic administration of bacteria results in their selective colonization of tumors, providing a convenient opportunity for tumor drug delivery.”
In fact, bacterial cancer therapy is not a new idea: In the 1890s, William Coley, a New York City surgeon, demonstrated that injection of live streptococcal organisms into cancer patients could shrink tumors. While his method was never widely adopted because radiotherapy was discovered at around the same time and antibiotics were not widely available, physicians have for decades been using a tuberculosis vaccine, bacillus Calmette–Guérin (BCG), as a therapy for bladder cancer.
The Danino lab has pioneered the strategy of using engineered bacteria for cancer therapy, with the development of methods to characterize different strains of bacteria, therapeutics, and genetic control circuits for effectively releasing cancer drugs. For their newly reported study, led by PhD student Candice Gurbatri, the investigators looked to engineer a translational therapeutic platform that improved upon a previous lysis circuit, and which would produce and release anti-PD-L1 and anti-CTLA-4 nanobodies directly in tumors. “Specifically, we coupled immunotherapeutic expression to an optimized lysing mechanism such that probiotic bacteria carrying the nanobodies home to the necrotic tumor core, grow to a critical density, and lyse, effectively releasing the therapeutics continuously within the tumor microenvironment.”
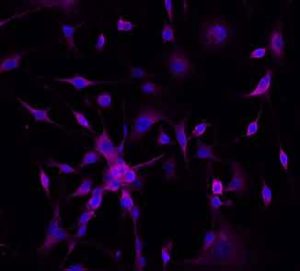
The scientists designed nanobodies targeting PD-L1 and CTLA-4, and having confirmed that the nanobodies would bind to their relevant targets, they cloned the sequences into plasmids, which were transferred into the widely used E. coli Nissle 1917 probiotic strain. “E. coli Nissle 1917 was chosen as a therapeutic vehicle for its proven safety, as it is currently prescribed for oral administration in humans, as well as its ease in genetic manipulation for the delivery of cancer therapeutics,” they wrote.
The team separately harnessed computational modeling techniques to scan multiple parameters and identify the optimal circuit variants to optimize drug release within the tumor. They integrated this optimized circuit into the genome of the E.coli Nissle 1917 strain, resulting in a strain that they called SLIC (synchronized lysing integrated circuit). The SLIC probiotic strain was naturally capable of finding and growing within tumors in the body, and the genomic integration of this circuit ensured greater stability of the system and higher levels of therapeutic release.
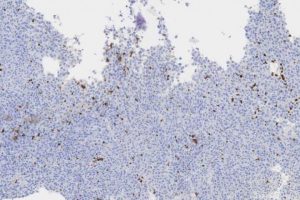
The research team used the probiotic delivery system to release nanobodies blocking PD-L1 and CTLA-4 within tumors in mouse models of lymphoma and colorectal cancer. Both tumor types are known to express these checkpoints to stop the immune system, from functioning properly. The strategy of blocking PD-L1 and CTLA-4 aims to remove the immune system brakes and enable T cells to attack the cancer.
Direct comparison studies in mice showed that a single dose of the SLIC probiotic system was more effective than clinically relevant anti-PD-L1 and anti-CTLA-4 antibodies, leading to complete tumor regression and preventing metastasis in early and late-stage mouse models of lymphoma. “We observed a markedly enhanced effect of our probiotic system, resulting in tumor clearance and prolonged survival when compared to animals treated with the antibody combination,” the scientists wrote. “We hypothesize that the observed therapeutic difference between the antibody and probiotic therapies is due to the probiotic’s ability to continuously antagonize CTLA-4 and PD-L1 intratumorally, thereby circumventing the need for the multiple injections vital for antibody therapy success.”
The researchers also tested the system for treating colorectal cancer, which has been less responsive to traditional immunotherapies. “Because of its local delivery, bacterial therapy may be used to deliver multiple therapeutics at once without increasing toxicities—a task currently difficult to achieve clinically with antibodies due to systemic toxicity,” the scientists wrote.
To treat this colorectal cancer mouse model, they paired the immune checkpoint nanobody SLIC system with a SLIC cytokine system (SLIC:GM-CSF), to further stimulate the immune system. Their experiments showed that a single dose of the probiotic cocktail resulted in tumor regression, with no observed side effects. “ … we observed an enhanced antitumor effect when compared to the monotherapies and a greater survival benefit,” the researchers noted. “The improved therapeutic outcome suggested a useful combination of these three therapeutics that is well tolerated by mice, as was evidenced by the maintenance of health and body weight.” The authors suggested that it should be possible to adapt the SLIC system to generate a wide variety of immunotherapeutics and test different combinations.
The team concluded, “The SLIC system should help advance the cancer immunotherapy field by providing a durable delivery vehicle in which combination therapies can be easily explored, therapeutic production is sustained, and toxicities are minimized for improved checkpoint blockade delivery to a broader range of cancer patients.”






