With the right improvement, the CRISPR gene editing system could revolutionize gene therapy. For example, CRISPR needs to introduce fewer off-target effects, not to mention fewer deleterious on-target effects. But even if CRISPR is on target and exerts the desired effect, there remains another problem: efficiency. Fortunately, CRISPR efficiency may be easily improved, report scientists based at UT Southwestern Medical Center. Just adjust the doses of the key CRISPR components—Cas9 protein and guide RNA (gRNA).
The UT Southwestern scientists hit upon their simple efficiency-boosting strategy while they were working on a gene therapy for Duchenne muscular dystrophy (DMD). Through trial and error, the scientists found that using a 10-to-1 ratio of gRNA to Cas9 allowed for optimal editing of a key DMD gene defect, the exon 44 deletion mutation. Compared to a 1-to-1 ratio, the scientists determined, the 10-to-1 ratio increased efficiency about 10-fold.
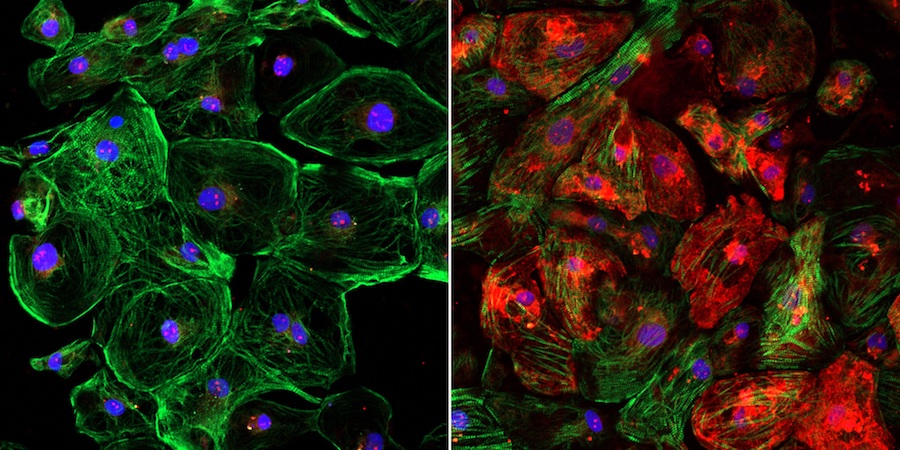
Detailed findings of the scientists’ work appeared March 6 in the journal Science Advances, in an article titled, “CRISPR-Cas9 corrects Duchenne muscular dystrophy exon 44 deletion mutations in mice and human cells.” The article describes how the scientists corrected the exon 44 deletion in patient-derived induced pluripotent stem cells, as well as in a new mouse model harboring the same deletion. Although the current study focuses on DMD, the study’s results could have implications for optimizing gene therapies for diseases other than DMD.
“Using AAV9 encoding Cas9 and single guide RNAs, we also demonstrate the importance of the dosages of these gene editing components for optimal gene correction in vivo,” the article’s authors wrote. “We also show that single guide RNAs, unexpectedly, are limiting for optimal gene editing in vivo and that editing efficiency can be enhanced ~10-fold by optimizing the dose of AAVs encoding Cas9 and single guide RNAs.”
The UT Southwestern scientists, led by Eric Olson, PhD, professor and chair, molecular biology, developed a method to edit the defective portion of the dystrophin gene by loading Cas9 into an adeno-associated virus (AAV), a harmless virus that is used to deliver the editing components into the cells. The guide RNA is also loaded into an AAV to direct Cas9 to the mutation where it snips the DNA.
The editing process bypasses the mutation and enables muscle fibers to produce dystrophin, with positive results documented in previous studies by Olson in large mammals, mice, and human cells.
In those studies, the team used a standard 1-to-1 ratio of Cas9 and guide RNA to help restore dystrophin production in muscle to more than 90% of normal.
In the new study targeting a different part of the gene, they discovered the 1-to-1 ratio didn’t work as well: Dystrophin production was only restored to 5% of normal when delivered into the bloodstream.
The scientists found using a 10-to-1 ratio of guide RNA to Cas9 allowed for optimal editing of that particular segment of the dystrophin gene. Within four weeks of a CRISPR dose, dystrophin production was restored in about 90% of muscle and heart fibers in mice with a common DMD mutation.
“This is surprising,” said Yi-Li Min, the study’s first author. “We had always delivered the guide RNA and Cas9 using two viruses in equal amounts and hadn’t thought to look into changing the ratio.”
DMD, the most common fatal genetic disease in boys, leads to muscle and heart failure, and premature death by the early 30s. Patients are forced into wheelchairs as their muscles degenerate and eventually onto respirators as their diaphragm muscles weaken. No effective treatment exists, though scientists have known for decades that a defect in any of the 79 exons that comprise the long dystrophin gene causes the condition.
Olson has published multiple studies in which his lab made single cuts at strategic points of DNA to correct mutations. Including his latest study that focused on deletion of exon 44, his lab has created CRISPR techniques that target the five most common defects seen in DMD patients, accounting for about half of cases worldwide. A clinical treatment for exon 44, which is located in one of the most common mutational hotspots on the gene, may benefit about 12% of patients.
The techniques have not yet been approved for clinical use, but Olson’s team took a major step toward that goal last year after publishing a Science study showing that CRISPR edits on exon 51 halted the progression of DMD in dogs.
Within several weeks of the gene editing, the missing protein was restored in muscle tissue throughout the body, including 92% correction in the heart and 58% in the diaphragm, the main muscle needed for breathing. Scientists have estimated a 15% threshold is needed to significantly help patients.
The lab is conducting longer-term studies in dogs to measure whether the dystrophin levels remain stable and to ensure the gene edits do not have adverse side effects.
Olson hopes the next step beyond dogs is a clinical trial, which would be among several that UT Southwestern’s gene therapy program aims to launch in the coming years to address numerous deadly childhood diseases.
“We have more to do before we can use this clinically,” Olson said, “but it’s exciting to see how far we’ve come.”
“As we test CRISPR on other defective parts of the dystrophin gene, it may be important to tweak our formulas for optimal results,” Olson added. “This new insight further facilitates the use of CRISPR as a therapy for Duchenne and perhaps a number of other diseases.”