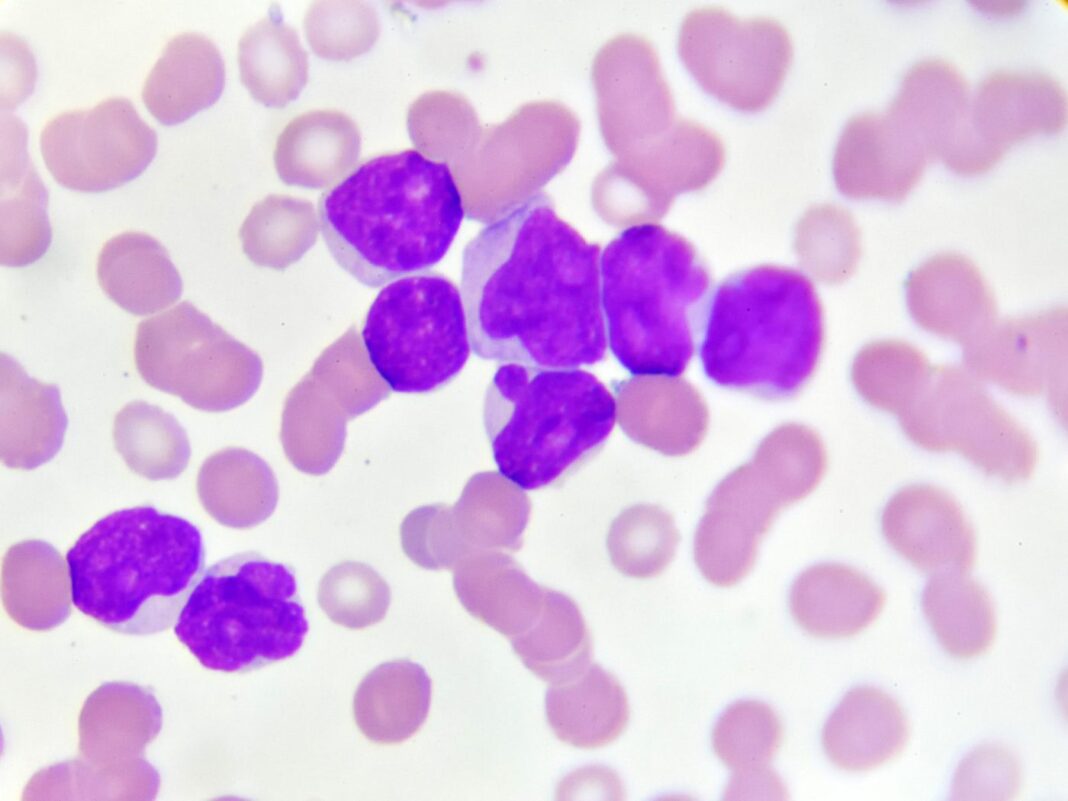
Acute myeloid leukemia (AML) starts in the bone marrow, but often moves into the blood, as well. AML develops as the consequence of a series of genetic changes in a hematopoietic precursor cell. These changes alter normal hematopoietic growth and differentiation, resulting in an accumulation of large numbers of abnormal, immature myeloid cells in the bone marrow and peripheral blood. Previous studies in mice suggest that AML cells inhibit healthy hematopoietic stem and progenitor cells (HSPCs). A new study demonstrates how secreted cell factors, in particular a protein called transforming growth factor beta 1 (TGFβ1), leads to a breakdown of hematopoiesis in humans. The findings suggest that blocking TGFβ1 could improve hematopoiesis in AML patients.
Their findings are published in the journal STEM CELLS in a paper titled, “Acute myeloid leukemia-induced functional inhibition of healthy CD34+ hematopoietic stem and progenitor cells.”
“AML is characterized by an expansion of leukemic cells and a simultaneous reduction of normal hematopoietic precursors in the bone marrow (BM) resulting in hematopoietic insufficiency, but the underlying mechanisms are poorly understood in humans,” wrote the researchers. “Assuming that leukemic cells functionally inhibit healthy CD34+ HSPCs via humoral factors, we exposed healthy BM-derived CD34+ HSPCs to cell-free supernatants derived from AML cell lines as well as from 24 newly diagnosed AML patients.”
The researchers at Heinrich-Heine-University Düsseldorf sought to determine what role fluids secreted by leukemic cells might play in inhibiting the growth of healthy HSPCs.

“Experiments using conditioned media (CM) from AML cells to address secretory mechanisms have been performed before, but mainly in mice. In order to gain new insights into how this plays out in humans, we focused on the interaction between leukemic cells and healthy HSPCs using an in vitro system modeling the in vivo situation of bone marrow infiltration by AML cells,” explained the study’s author, Thomas Schroeder, MD, PhD, department of hematology, oncology, and clinical immunology.
“We focused on secreted factors from AML cells as a major mechanism causing hematopoietic failure based on the assumption from previous reports,” wrote the researchers. “Our results show that AML cells functionally impair healthy hematopoietic cells in terms of cell production, cell cycle, colony forming capacity, and in particular erythroid differentiation. This functional impairment was reflected on the molecular level by a specific gene expression signature. Molecular as well as functional analyses identified TGFβ1 as one relevant trigger factor and potential therapeutic target.”
Their findings revealed that exposure to AML-derived supernatants significantly inhibited proliferation, cell cycling, colony formation, and differentiation of healthy CD34+ HSPCs.
“Blocking the TGFβ1 pathway is something that could be pharmacologically accomplished with a TGFβ1 inhibitor such as SD208. Our data indicate this could be a promising approach to improve hematopoiesis in AML patients,” added Schroeder.
Jan Nolta, PhD, editor-in-chief of STEM CELLS, commented, “Finding factors for possible intervention in the perplexing issue of suppression of normal hematopoiesis by AML cells is highly important. The possibility of targeting TGFβ1 in order to allow the normal stem and progenitor cells to expand is a promising lead toward future treatments.”