A research team headed by scientists at the University of Edinburgh, and at Jagiellonian University Medical College, has for the first time identified specific regions of the brain that are damaged by high blood pressure (BP) and may contribute to a decline in mental processes and the development of dementia.
The study evaluated combined data from brain magnetic resonance imaging (MRI) studies, genetic analyses and observational data from thousands of patients, to look at the effect of high blood pressure on cognitive function. Tomasz Guzik, MD, PhD, Professor of Cardiovascular Medicine, at the University of Edinburgh (UK) and Jagiellonian University Medical College, Krakow (Poland), who led the research, said: “By using this combination of imaging, genetic and observational approaches, we have identified specific parts of the brain that are affected by increases in blood pressure, including areas called the putamen and specific white matter regions … We hope that our findings may help us to develop new ways to treat cognitive impairment in people with high blood pressure.”
“Studying the genes and proteins in these brain structures could help us understand how high blood pressure affects the brain and causes cognitive problems. Moreover, by looking at these specific regions of the brain, we may be able to predict who will develop memory loss and dementia faster in the context of high blood pressure. This could help with precision medicine, so that we can target more intensive therapies to prevent the development of cognitive impairment in patients most at risk.”
Guzik and colleagues reported on their findings in European Heart Journal, in a paper titled “Genetic analyses identify brain structures related to cognitive impairment associated with elevated blood pressure.”
High blood pressure occurs in 30% of people worldwide, with an additional 30% showing initial stages of the disease. Studies have shown that high blood pressure can affect how well the brain works and that it can cause long-term changes, the authors noted. “Observational and prospective studies, as well as randomized clinical trials of antihypertensive therapies, have demonstrated that hypertension may be causally associated with impaired cognitive performance.” However, it hasn’t been known exactly how high blood pressure damages the brain ,and which specific regions are affected. “Therefore, it is of primary clinical importance to identify specific brain areas mediating BP-dependent cognitive changes,” the investigators continued.
For their newly reported study, Guzik and an international team of researchers designed what they termed “a triangulation approach to identify brain structures potentially responsible for the effects of BP on cognitive function.” To do this they evaluated brain MRI imaging data from over 30,000 participants in the UK Biobank, together with genetic information from genome-wide association studies (GWAS) from UK Biobank and two other international groups (COGENT and the International Consortium for Blood Pressure).They applied Mendelian randomisation (MR) analyses to see if high blood pressure was actually the cause of changes to specific parts of the brain rather than just being associated with these changes. The authors further explained, “Firstly, we comprehensively mapped brain structures potentially influenced by BP in midlife using MR analysis. Secondly, we elucidated the effects of BP on cognitive function in well-powered datasets. Finally, using MR analysis, we identified structures in the brain that accompany the detrimental effects of elevated BP on cognitive function in humans.
Guzik commented, “Mendelian randomization is a way of using genetic information to understand how one thing affects another. In particular, it tests if something is potentially causing a certain effect, or if the effect is just a coincidence. It works by using a person’s genetic information to see if there is a relationship between genes predisposing to higher blood pressure and outcomes. If there is a relationship, then it is more likely that the high blood pressure is causing the outcome. This is because genes are randomly passed down from parents, so they are not influenced by other factors that could confuse the results. In our study, if a gene that causes high blood pressure is also linked to certain brain structures and their function, then it suggests that high blood pressure might really be causing brain dysfunction at that location, leading to problems with memory, thinking and dementia.”
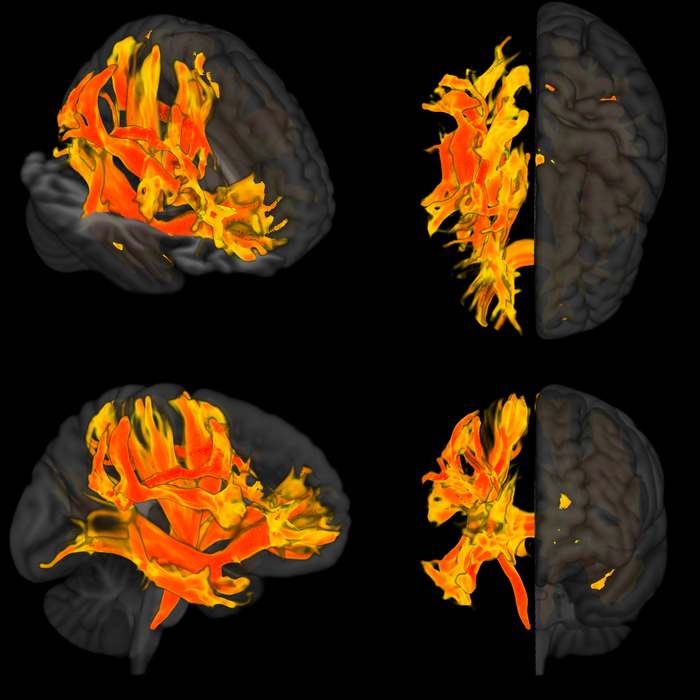
Through their work the researchers found that changes to nine parts of the brain were related to higher blood pressure and worse cognitive function. These regions included the putamen, which is a round structure in the base of the front of the brain, responsible for regulating movement and influencing various types of learning. Other areas affected were the anterior thalamic radiation, anterior corona radiata and anterior limb of the internal capsule, which are regions of white matter that connect and enable signaling between different parts of the brain. The anterior thalamic radiation is involved in executive functions, such as the planning of simple and complex daily tasks, while the other two regions are involved in decision-making and the management of emotions.
The changes to these areas included decreases in brain volume and the amount of surface area on the brain cortex, changes to connections between different parts of the brain, and changes in measures of brain activity. The team then validated their findings in an independent cohort of patients. “The pattern of brain damage linked to BP by genetic causal inference methods was then validated in an independent, well-phenotyped, prospectively recruited cohort,” they stated.
Guzik added, “We thought these areas might be where high blood pressure affects cognitive function, such as memory loss, thinking skills and dementia. When we checked our findings by studying a group of patients in Italy who had high blood pressure, we found that the parts of the brain we had identified were indeed affected.”
Study first author Mateusz Siedlinski, PhD, at the Jagiellonian University Medical College, said, “Our study has, for the first time, identified specific places in the brain that are potentially causally associated with high blood pressure and cognitive impairment. This was uniquely possible thanks to the availability of data from UK Biobank, including MRI brain images, and thanks to previous research identifying genetic variants that affect the structure and function of over 3000 areas of the brain.”
In their discussion, the authors noted that the study supports the existence of a “modest, potentially causal, detrimental effect,” of higher systolic blood pressure, and pulse pressure (PP), but not diastolic blood pressure, on cognitive performance in midlife, which they say “may serve as additional evidence regarding the role of hypertension in dementias.”
Co-author Joanna Wardlaw, PhD, head of Neuroimaging Sciences at the University of Edinburgh, further commented, “It has been known for a long time that high blood pressure is a risk factor for cognitive decline, but how high blood pressure damages the brain was not clear. This study shows that specific brain regions are at particularly high risk of blood pressure damage, which may help to identify people at risk of cognitive decline in the earliest stages, and potentially to target therapies more effectively in future.”
The authors acknowledged limitations of the study, pointing out that participants in the UK Biobank study are mainly white and middle-aged, so it might not be possible to extrapolate the findings more generally to other populations, including to older people. However, they concluded, “While clinical trials targeting specific brain structures may be challenging, focused imaging of these structures in future preclinical and clinical studies may, in due course, support a more personalized approach to hypertensive patients in relation to cognitive impairment. It may be possible that identification of imaging-derived phenotypes associated with hypertension and cognitive impairment can guide the choice of imaging surrogate biomarkers in future clinical studies of antihypertensive therapies.”
An accompanying editorial Ernesto Schiffrin, MD, PhD, from Sir Mortimer B. Davis-Jewish General Hospital and McGill University, Montreal, (Canada), and James Engert, PhD, from the McGill University Health Centre Research Institute, Montreal, note that “Further mechanistic studies of the effects of BP [blood pressure] on cognitive function are required to determine precise causal pathways and relevant brain regions.”
Highlighting one of the study’s findings about systolic and diastolic blood pressure, Shiffrin and Engert wrote, “Perhaps one of the more interesting results in this study is the possible distinct causal effects of SBP vs. DBP. The authors observed some overlapping results for SBP and DBP on cognitive function when analysed in isolation. However, when each parameter is analysed after adjusting for the other, or in multivariable models, intriguing findings begin to emerge. DBP alone does not predict a decline in cognitive function, but in fact, is protective when adjusted for SBP. This result was true both observationally and when using Mendelian randomisation.”