Scientists at the Diabetes Research Institute (DRI), University of Miami, have identified and characterized a population of progenitor cells located in defined areas of the human pancreas, which can be stimulated to develop into glucose-responsive beta cells. The researchers, co-led by Juan Dominguez-Bendala, Ph.D., DRI director of pancreatic stem cell development for translational research, and Ricardo Pastori, Ph.D., director of molecular biology, claim that their discovery could feasibly allow the development of cell-based therapies for type 1 and type 2 diabetes that are derived from the patients’ own stem cells.
“Our in-depth study of these pancreatic stem cells may help us tap into an endogenous cell supply 'bank' for beta-cell regeneration purposes and, in the future, lead to therapeutic applications for people living with type 1 diabetes,” said and co-principal investigator of the team’s research, which is published in Cell Reports (“P2RY1/ALK3-Expressing Cells within the Adult Human Exocrine Pancreas Are BMP-7 Expandable and Exhibit Progenitor-like Characteristics”).
The existence of progenitor-like cells in the adult human pancreas has been “hypothesized for decades, but their characterization has proven elusive,” the authors explain. “The study of their nature and potency may help us tap into an endogenous cell repository for pancreatic β cell regeneration, which could lead to therapeutic applications for type 1 and type 2 diabetes.”
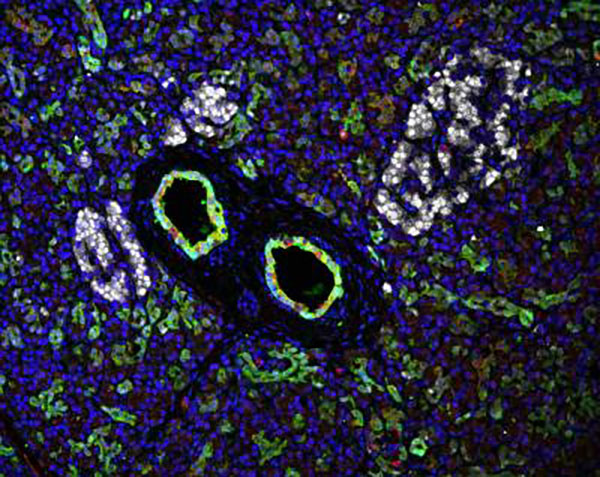
The team’s previous work had shown that the FDA-approved growth factor bone morphogenic protein 7 (BMP-7) stimulated progenitor-like cells in cultured human nonendocrine pancreatic tissue. Their latest studies have demonstrated that BMP-7-responsive progenitor cells are located in the nonendocrine pancreatic ducts and pancreatic duct glands of the pancreas, but not in the pancreatic islets themselves. The progenitors were found to express PDX1, which is required for beta-cell development, and the cell-surface receptor ALK3, which is associated with regeneration in different tissue types.
Using both ALK3 and the cell-surface receptor P2RYI as a surrogate for PDX1 (which is a nuclear protein), the researchers were then able to sort and culture the progenitor cells. Exposing the cells to BMP-7 resulted in upregulation of pancreatic progenitor genes, while withdrawing BMP-7 led to an increase in the expression of endocrine differentiation markers. RNA sequence analysis and other data indicated that “BMP-7 engages the cell division-ready phenotype,” of the cells, and that subsequent withdrawal of BMP-7 induces cell-cycle arrest and multilineage differentiation. Essentially, administration of BMP-7 followed by its withdrawal triggered the cells to proliferate and then to differentiate. “Together with our previous findings using BMP-7 to stimulate their growth, we believe that we may be able to induce these stem cells to become functional islets,” Dr. Pastori comments.
Type 1 diabetes insulin-producing cells in the pancreatic islets are destroyed by the patient's own immune system. Islet transplantation using donor cells has been used successfully in some type 1 diabetes patients, but there aren’t enough donor cells available to treat every patient. In the search for alternative sources of cells for transplantation, research has focused primarily on embryonic stem cells, induced pluripotent stem cells, adult stem cells, and porcine islets.
The discovery of pancreatic progenitors could instead allow the development of new approaches that trigger regeneration of the patient’s own insulin-producing cells. However, scientists may still need to develop methods to prevent the regenerated cells from autoimmune-related destruction in type 1 diabetes patients.
“Our findings go well beyond the comprehensive characterization of this progenitor cell population,” the authors write. “The identification of their anatomical niche will allow us to screen for their existence in the exocrine pancreas of both type 2 and type 1 diabetes patients. Provided that these cells remain intact after the autoimmune destruction of β cells in type 1 diabetes, their responsiveness to BMP-7 (a Food and Drug Administration [FDA]-approved agent) could be potentially used to restore β cell mass in situ in the context of concomitant interventions to quell autoimmunity.”
“The ability to offer regenerative medicine strategies to restore insulin production in the native pancreas could one day replace the need for transplantation of the pancreas or insulin-producing cells,” comments Camillo Ricordi, M.D., director of the DRI and Stacy Joy Goodman Professor of Surgery. “In type 1 diabetes, this would require abrogation of autoimmunity to avoid immune destruction of the newly formed insulin producing cells. For this reason, our current efforts are converging on immune tolerance induction without the need for life long antirejection drugs.”