New three-dimensional culturing, structuring, and analytical techniques will revolutionize early-phase drug development. These techniques promise to outperform the traditional technique, the use of a two-dimensional monolayer, in gauging the potential for interactions between candidate drugs and dysfunctional organs. Although two-dimensional models can provide an indication of safety and even hint at therapeutic efficacy, they are not truly representative of the organs from which they are derived.
Their major shortcoming is the lack of context. Cells grown in culture in a two-dimensional monolayer lack the stoma—the connective tissue—that gives the parent organ its structure. Moreover, organs are composed of multiple cell types that interact with one another, the surrounding environment, and any medicines to which they are exposed. Single cells in two-dimensional monolayers can therefore never fully replicate how a diseased organ will react to treatment.
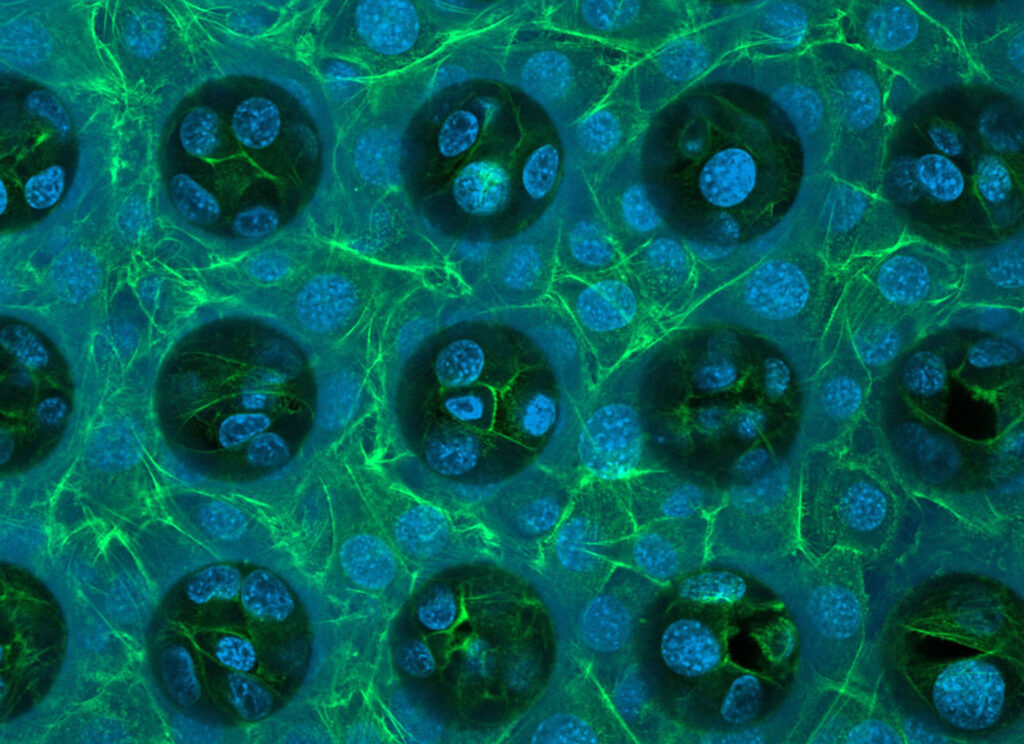
In the past few decades—as indicated in a recent review article (Corrò et al. Am. J. Physiol. Cell Physiol. 2020; 319(1): C151–C165)—novel culturing and manufacturing techniques and hydrogel scaffolds have given researchers the tools to create miniature, three-dimensional versions of organs called organoids. These models have both the composition and the three-dimensional structure of the source organ.
Shedding light on bioinks
The new techniques and materials may be employed in additive, or bottom-up, manufacturing processes. For example, three-dimensional printing techniques may be used to build organoids layer by layer. The ability to combine cells and support structures has been a revelation, says Isabella Bondesson, field application scientist, Cellink.
“3D bioprinting is biology’s version of 3D printing, where the printing method has been optimized to work with cell-friendly materials and gentle conditions to maintain cell viability through the printing process,” she elaborates. “With 3D bioprinting, living cells are embedded in a matrix, called the bioink, and then arranged into a 3D structure.
“The bioink is usually some sort of hydrogel designed to mimic the extracellular matrix for the tissue of interest, providing the right properties for the embedded cells to proliferate, migrate, and mature within the 3D model. This allows researchers to recreate cellular environments and tissue structures, as different cells and tissue environments can be combined and positioned in relation to each other as they would be structured in vivo.”
Several refined forms of bioprinting techniques have been introduced. One of them is light-based bioprinting, a method for using light patterns to shape 3D structures. This method has the potential to make organoids even more representative of real tissues.
“In light-based bioprinting, the bioink is cured with visible light to maintain cell viability,” Bondesson details, “and as the light pattern is exposed onto cell-laden material, the exposed volumes of bioink are cured. The benefit is that you can get extremely high resolution and precision. With digital light projection, you can form shapes with a resolution down to around 10 µm, and with two-photon polymerization, you can achieve submicron resolution.
“It is also a gentle printing method where stiffness and shape easily can be altered. The only caveat to light-based bioprinting is that you must work with bioinks that are curable with light, which means that you have slightly less freedom in combining multiple materials.”
As bioprinting techniques improve, bioprinting applications grow more sophisticated. According to Bondesson, the bioprinting sector has been working to develop systems tailored to the needs of drug makers. She notes, “Part of these efforts have focused on software development. When coding becomes unnecessary for bioprinter operation, anyone working in cell biology can easily enter the world of bioprinting.”
“Such advancements have allowed for greater inroads into the biopharma industry,” she continues. “When biopharma researchers gain the ability to develop more standardized 3D models, like organoids, they can dramatically accelerate their drug discovery processes and help bring novel treatments to market more quickly.”
Characterizing 3D cultures
In the biopharma industry, applications of 3D bioprinting have become commonplace, observes Simone Pasqua, the founder and marketing director of CellDynamics. He credits the expansion of 3D bioprinting to the availability of analytical technologies that facilitate the characterization of 3D cellular models.
“Until a few years ago, the use of 3D biology was confined to a few cutting-edge institutes where the foundations were laid,” he says. “But in the space of a few years, we have seen a profound transformation. Today, 3D cellular models are our daily bread.”
Pasqua notes that CellDynamics’ focus is on developing technologies that “recognize the complexities introduced by the third dimension” and are able to characterize 3D cultures—including organoids—in great detail. “Until a few years ago, parameters such as mass density and weight were completely underestimated,” he adds. “Today, we can no longer permit this.
“We believe that incorporating new quantitative outputs such as surface accessible area, sphericity index, and shape reconstruction will significantly enrich the information we have at our disposal. Our aim is to harness this data to create intelligent algorithms that effectively normalize the variability introduced by the third dimension.”
This view is shared by D. Andrea Cristaldi, PhD, senior R&D specialist at CellDynamics. He emphasizes that the company’s focus on model characterization reflects the priorities of the biopharma industry: “The concept and rationale of our technology have been established through extensive feedback from researchers over several years, with the objective of introducing novel metrics to consider when dealing with 3D cell culture.”
“While many concentrate on size-related outputs, the inclusion of the third dimension necessitates careful consideration as samples with similar sizes often present significant cross-sectional differences that cannot be underestimated,” he continues. “We have addressed this gap by conceiving and developing a benchtop automated technology that permits researchers to obtain a distinct and comprehensive understanding of their 3D cell cultures via a tailored biophysical characterization.”

Cristaldi points to CellDynamics’ W8 system, which he describes as a “biophysical characterization tool for 3D cellular models.” He explains that the technology was developed with the specific needs of drug developers in mind.
“We addressed all the needs researchers have highlighted during the past years of R&D,” Cristaldi asserts. “The W8 ensures low sheer stress levels, preserves sample viability, maintains sterility, and permits a label-free analysis.
“We firmly believe that helping users to answer everyday workflow questions is key. For example, users need to know if drug activity is low or high because of the intrinsic properties of the drug, or because of influences such as the microenvironment, the extracellular matrix, or the stroma.”
According to Pasqua, the ability to analyze mass density information is a major advantage. “Mass density insights offer a unique window into the compactness or stiffness of organoids,” he insists. “These are crucial variables that exert a direct influence on the permeation of treatments within these complex structures. This knowledge serves as a cornerstone for refining drug delivery strategies, guaranteeing that therapeutic agents reach their target cells effectively within the organoid structure, and advancing the precision and efficacy of drug development efforts.”
Patient-specific models
The demand for organoids will be further stimulated by growth in the personalized medicine sector, says Robert Vries, PhD, the CEO of HUB Organoids. The company, formerly known as Hubrecht Organoid Technology, indicates that it generates patient-derived organoids (PDOs)—or “mini-organs in a dish”—from adult epithelial stem cells.
“PDOs are three-dimensional models of human organs that are grown in the laboratory using tissue samples obtained directly from patients,” Vries explains. “They recapitulate the structure and function of the original organs and are currently being used to better understand human diseases and to develop and test new therapeutics. The use of human models that represent real patients results in a higher success of drug development and faster development of new treatments to patients in the clinic.”
According to Vries, HUB Organoid’s approach has a number of advantages over other production methods. “We start from patient resections or biopsies,” he details. “Depending on the organ of origin, we have optimized specific methods and cocktails of growth factors that make up the culture media to support the survival, proliferation, and differentiation of adult epithelial stem cells, resulting in organoids that grow and self-assemble without the need for any other external intervention. No genetic modifications or mechanical forces are required.”
“The organoids keep all the genetic and functional features of the original cells,” Vries asserts. “Because of this, the organoids can directly and functionally represent patients.”
“The only other option for developing organoids in the laboratory is to use induced pluripotent stem cells (iPSCs) as starting material,” he maintains. “iPSCs are derived from skin or blood cells, and the process of developing organoids from iPSCs is typically lengthier than from adult epithelial stem cells, requires multiple steps, and results in less robust and stable cultures.”


