Obesity has become a worldwide epidemic, dramatically increasing the incidence of disorders including type 2 diabetes, nonalcoholic fatty liver disease, and other cardiometabolic abnormalities. While lifestyle factors such as diet and exercise play a role in the development and progression of obesity, scientists have come to understand that obesity is also associated with intrinsic metabolic abnormalities, including mitochondrial dysfunction. Murine studies by an international research team headed by researchers at the University of California (UC), San Diego, School of Medicine have now shed new light on how obesity affects mitochondria, the all-important energy-producing structures of our cells.
The scientists found that when mice were fed a high-fat diet, mitochondria within the animals’ fat cells broke apart into smaller mitochondria with reduced capacity for burning fat. The study results also showed that this process is controlled by a single gene, RalA, and that deleting the gene in mice fed a high-fat diet protected them from excess weight gain.
“Caloric overload from overeating can lead to weight gain and also triggers a metabolic cascade that reduces energy burning, making obesity even worse,” said research lead Alan Saltiel, PhD, professor in the department of medicine at UC San Diego School of Medicine. “The gene we identified is a critical part of that transition from healthy weight to obesity … In essence, chronic activation of RalA appears to play a critical role in suppressing energy expenditure in obese adipose tissue. By understanding this mechanism, we’re one step closer to developing targeted therapies that could address weight gain and associated metabolic dysfunctions by increasing fat burning.”
Saltiel and colleagues reported on their studies in Nature Metabolism, in a paper titled, “Obesity causes mitochondrial fragmentation and dysfunction in white adipocytes due to RalA activation.”
Obesity, which affects more than 40% of adults in the United States, occurs when the body accumulates too much fat, which is primarily stored in adipose tissue. Adipose tissue normally provides important mechanical benefits by cushioning vital organs and providing insulation. It also has important metabolic functions, such as releasing hormones and other cellular signaling molecules that instruct other tissues to burn or store energy.
In the case of caloric imbalances like obesity, the ability of fat cells to burn energy starts to fail, which is one reason why it can be difficult for people with obesity to lose weight. How these metabolic abnormalities start is among the biggest mysteries surrounding obesity.
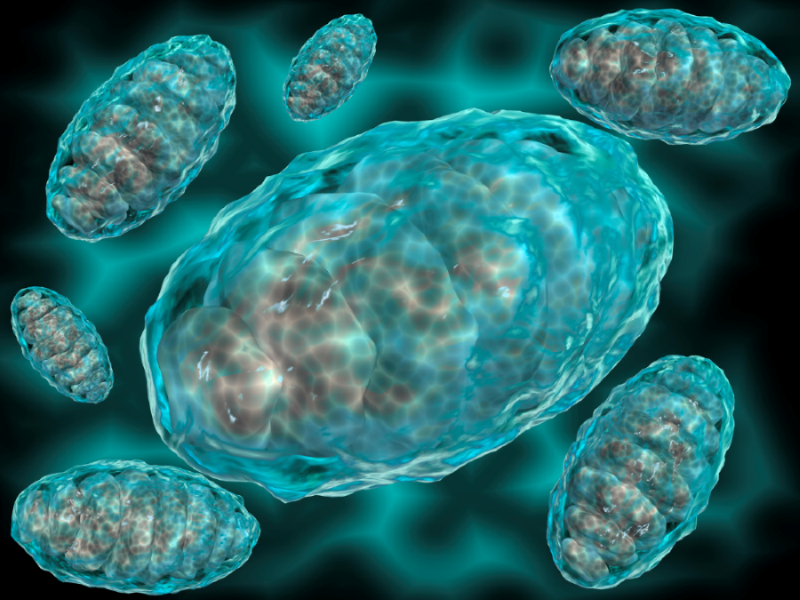
To answer this question, Saltiel and colleagues looked more closely at the link between obesity and mitochondria in a fat cells. “Mitochondrial dysfunction is a characteristic trait of human and rodent obesity, insulin resistance, and fatty liver disease,” the team wrote. “While mitochondria play an important metabolic role in healthy adipocytes, oxidizing fuel to produce ATP and generating heat during thermogenesis, mitochondrial function is impaired in obese individuals; however, what drives mitochondrial damage and how it contributes to obesity and its many complications remains unknown.”
For their reported studies the team fed mice a high-fat diet and measured the impact of this diet on mitochondria in the animals’ white adipocytes. They discovered an unusual phenomenon. After consuming a high-fat diet, mitochondria in parts of the mice’s adipose tissue underwent fragmentation, splitting into many smaller, ineffective mitochondria that burned less fat.
They also discovered that this metabolic effect was driven by the activity of a single molecule, called RalA. “… we show that high-fat diet (HFD) feeding causes mitochondrial fragmentation in inguinal white adipocytes from male mice, leading to reduced oxidative capacity by a process dependent on the small GTPase RalA,” the team continued. “RalA expression and activity are increased in white adipocytes after HFD.”

The authors further noted, “Thus, chronic activation of RalA plays a key role in repressing energy expenditure in obese adipose tissue by shifting the balance of mitochondrial dynamics toward excessive fission, contributing to weight gain and metabolic dysfunction.”
The researchers also showed that by deleting the RalA gene they were able to protect the mice against diet-induced weight gain. “These beneficial effects of RalA deletion were driven by a reversal of the increased mitochondrial fission in white adipocytes induced by feeding mice HFD,” the team explained.
Further investigation indicated that some of the proteins affected by RaIA in mice are analogous to human proteins that are associated with obesity and insulin resistance, suggesting that similar mechanisms may be driving human obesity.