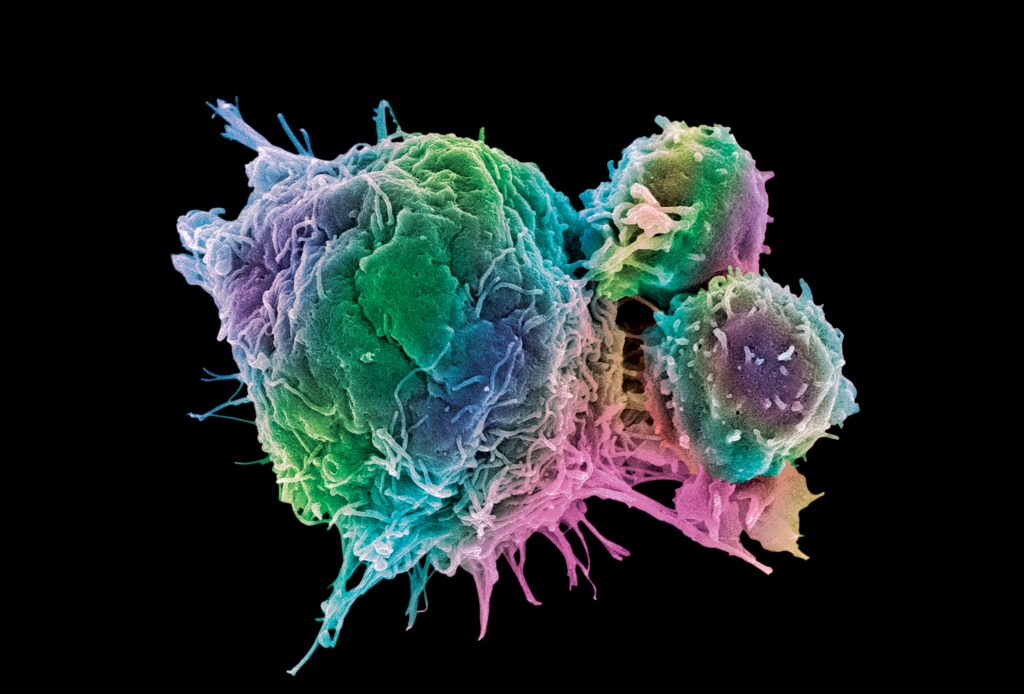
Cell therapy is an emerging form of treatment that is poised to revolutionize medicine. Several chimeric antigen receptor (CAR) T-cell therapies have been approved by the U.S. Food and Drug Administration for treating leukemia, and at least 500 other studies using CAR T cells for cancer treatment are under clinical trials. A year ago, Japan’s health ministry also approved the world’s first use of corneal cells reprogrammed from induced pluripotent stem cells (iPSCs) for therapy,1 paving the way for expanded use of iPSCs in clinics.
The process of cell manufacturing typically involves cell isolation and engineering before shipping cryopreserved cells from a centralized facility to clinics for infusion into patients. Technology for cryopreservation is hence critical to provide high-quality cells to achieve desirable clinical outcomes. Good materials and methods for cryostoring cells are equally pivotal to biobanking for maintaining human biospecimens such as tumor cells, umbilical cord blood, and tissue-derived stem cells, as well as excess engineered cells in cases when repeated doses are needed for efficacious therapies.
During the process of cryopreservation and thawing, cell viability can suffer due to reasons such as dehydration, toxic solute levels, formation of intracellular ice crystals, and osmotic stress.2 The most common protocol for cryostoring uses dimethyl sulfoxide (DMSO),3 a cell membrane–permeating cryoprotectant that reduces intracellular ice crystal formation. However, this comes with a trade-off as DMSO is known to induce oxidative stress and gene expression changes. This chemical can also damage organelles, cytoskeletons, and cell membranes, thus adversely affecting cell viability and functionality.4 It has been reported that the cell viability of thawed CAR T cells can be as low as 50% after cryopreservation with DMSO.5
Recently, a team of scientists from the National Institutes of Health (NIH) led by David Stroncek, MD, found that DMSO-cryopreserved CAR T cells displayed similar expansion capacity, transduction efficiency, and clinical outcomes to their fresh counterparts—however, the cryopreserved cells exhibited greater mitochondrial dysfunction, apoptotic signaling, and cell damage. Stroncek and colleagues stressed the need to better assess the clinical impact of cryopreservation-related microdamage.6 Previous reports had demonstrated that the in vivo therapeutic efficacy of cryopreserved natural killer (NK) cells is significantly lower than that of fresh NK cells.7 A similar finding emerged when cryopreserved and fresh mesenchymal stem cells were compared for their ability to inhibit T-cell proliferation in vitro.8
“Cryopreservation is absolutely essential to allow all release testing to be performed and for shipping CAR T-cell products,” argues Bruce L. Levine, PhD, a professor at the University of Pennsylvania. “There is a need for improved formulations with a lower percentage of DMSO that can enhance cell recovery and viability. DMSO-free formulations should also be considered for preserving CAR T cells.”
Although the use of fresh cellular materials may be advantageous and help to achieve better clinical outcomes, it can make manufacturing and logistics much more complex and expensive. Currently, cell therapies such as CAR T-cell treatments and their associated healthcare costs can be as high as $500,000 per patient,9 and medical literature has started referring to this problem as “financial toxicity.” Therefore, there is a strong demand for improved materials and methods for cryopreservation, and better means to assess the biological and clinical impacts of cryostorage to make cell manufacturing and therapy more efficient.
Emerging materials for cryopreservation and thawing
“With widespread application of cell therapy, cells have to be maintained at high viability and function at ambient, hypothermic, or cryogenic temperature for convenient and wide distribution to end users,” notes Xiaoming He, PhD, a professor at the University of Maryland. “Some ways to tackle this challenge include replacing toxic chemicals like DMSO and glycols with biocompatible materials like sugars as cryoprotective agents, encapsulating cells in hydrogels, and using nanomaterials.”
Inspired by the ability of tardigrades, or water bears, to survive freezing, the team led by Xiaoming He conjugated trehalose, a natural sugar that disrupts intracellular ice crystal formation, to nanoparticles that can be readily endocytosed by human stem cells. This technology overcomes the inability of trehalose to permeate the cell membrane and enables intracellularly available trehalose to confer cryoprotection.10 The same team also designed cold-responsive nanoparticles that release trehalose intracellularly upon cooling, and offers the additional benefit of skipping a cell washing step that can lead to cell loss.11
A group of researchers at the University of Warwick led by Matthew I. Gibson, PhD, also demonstrated that extracellular deposition of naturally occurring type III antifreeze proteins significantly improves the post-thaw recovery of cells seeded in a monolayer.12 Recently, Anne Meddahi-Pellé, MD, PhD, and her team from the University of Paris synthesized dextran-based hydrogels that demonstrated comparable cryoprotective ability as DMSO, without the side effects, albeit in human cell lines.13
According to David Stroncek from NIH, there is also a strong need for better thawing technology. “Thawing technology is important because thawing cells too slowly can damage cells, and once cells are thawed, DMSO is cytotoxic,” he points out. “The thawing process varies from center to center, but most protocols involve rapid thawing of the cells in a water bath with manual manipulation of the cells.”
Together with colleagues from China, Xiaoming He synthesized magnetic nanoparticles14 and made use of magnetic induction heating to more uniformly thaw stem cells. The nanomaterials provided a spatially homogenous warming rate during thawing, enabling faster and more uniform melting of ice crystals.
Remarkably, stem cells that were thawed using the nanoparticle technique exhibited higher viability and proliferative capacity while suffering minimal damage to their organelles, compared to their counterparts thawed using water baths. Crucially, the stem cells also better retained their ability to differentiate to different lineages, an important biological criterion for the use of stem cells in regenerative medicine. A similar result was reported by John Bischof, PhD, and his colleagues at the University of Minnesota.15 They made use of inductive heating of magnetic nanoparticles to minimize thermal mechanical stresses and improve cryopreservation of cells and tissues.
Assessing the impact of cryopreservation
“It is also crucial for biological materials to retain high viability, structural integrity, and functionality after cryopreservation and thawing,” maintains Xiaoming He.
Typically, assays measuring cell viability and metabolism are used to evaluate the impact of cryopreservation. However, these metrics provide little information about whether the critical polyfunctionalities of cells are affected.
For instance, while cell viability after cryopreservation may be high, the cytotoxic functions of CAR T cells or the regenerative capacity of stem cells may be altered. Hence, researchers are starting to assess the biological and clinical impacts of cryopreservation more comprehensively.
Gene expression change is an important metric because it provides a global view on the different gene pathways that are affected by cryopreservation and the extent to which they are being affected. A team led by Qing Ye, MD, PhD, from the Affiliated Hospital of Nanjing University Medical School found that different tissues and cells are affected differently by cold ischemia,16 which occurs to biological materials when they are denied their blood supply and chilled, until they are warmed by having their blood supply restored. The integrity of medium and long genomic DNA and of RNA was impacted by the length of cold ischemia time, with nucleic acids found in skin tissues being most resistant to degradation after isolation.
Aifen Lin, PhD, and her colleagues at the Wenzhou Medical University, examined the effects of −80°C storage on the quality of gastric tumor tissues.17 They found that the impact of storage duration on RNA integrity was minimal, but the composition of the tissue specimens, that is, the ratio of tumor to stromal cells (in particular, those with greater percentage of tumor cells), had better RNA quality after extraction. These results demonstrate the importance of performing quality control to accurately assess the impact of cryopreservation on gene expressions of different cell types used for therapy.
Application-specific assays are also crucial to determine whether cryopreserved cells are going to function therapeutically. For instance, Xiaoming He and his team administered several tests, including assessments of stem cell differentiation potential, to evaluate the impact of their magnetic nanoparticle heating technology.
Conclusions
The field of cell therapy is evolving rapidly with new therapeutic targets and with better techniques to transfect cells19 and enhance safety.20 As the population ages, the demand for cell-based regenerative medicine, biobanking, and tissue transplants is also likely to increase. These trends will intensify the need for better ways to characterize the impact of cryopreservation technology to improve cryostoring and thawing. Innovations in cryopreservation will also benefit biomedical research by enhancing current protocols and tools to preserve organoids21 and xenografts, which are becoming more popular in drug screening and basic science research.
References
1. Cyranoski, D. Woman is first to receive cornea made from ‘reprogrammed’ stem cells. Nature September 2, 2019.
2. Karlsson JOM, Toner M. Long-term storage of tissues by cryopreservation: critical issues. Biomaterials 1996; 17(3): 243–256.
3. Mandumpal JB, Kreck CA, Mancera RL. A molecular mechanism of solvent cryoprotection in aqueous DMSO solutions. Phys. Chem. Chem. Phys. 2019; 13: 3839–3842.
4. Best BP. Cryoprotectant Toxicity: Facts, Issues, and Questions. Rejuvenation Res. 2015; 18(5): 422–436. [Correction appears in Rejuvenation Res. 2018; 21(1): 87.]
5. Elavia N, McManus A, Highfill SL, et al. The Post-Thaw Recovery of Cryopreserved Chimeric Antigen Receptor (CAR) T-Cells during Manufacture Is Better Than That of Cryopreserved Peripheral Blood CD3+ Cells. Blood 2017; 130(Suppl. 1): 4475.
6. Panch SR, Srivastava SK, Elavia N, et al. Effect of Cryopreservation on Autologous Chimeric Antigen Receptor T Cell Characteristics. Mol. Ther. 2019; 27(7): 1207–1338.
7. Szmania S, Lapteva N, Garg T, et al. Ex vivo-expanded natural killer cells demonstrate robust proliferation in vivo in high-risk relapsed multiple myeloma patients. J. Immunother. 2015; 38(1): 24–36.
8. François M, Copland IB, Yuan S, et al. Cryopreserved mesenchymal stromal cells display impaired immunosuppressive properties as a result of heat-shock response and impaired interferon-γ licensing. Cytotherapy 2012; 14(2): 147–152.
9. Jayaraman K. Cut-price CAR-T cell therapies top India’s biotech agenda. Nat. Biotechnol. 2019; 37(12): 1388–1389.
10. Rao W, Huang H, Wang H, et al. Nanoparticle-mediated intracellular delivery enables cryopreservation of human adipose-derived stem cells using trehalose as the sole cryoprotectant. ACS Appl. Mater. Interfaces 2015;7(8):5017–28.
11. Zhang Y, Wang H, Stewart S, et al. Cold-Responsive Nanoparticle Enables Intracellular Delivery and Rapid Release of Trehalose for Organic-Solvent-Free Cryopreservation. Nano Lett. 2019; 19(12): 9051–9061.
12. Tomás RMF, Bailey TL, Hasan M, Gibson MI. Extracellular Antifreeze Protein Significantly Enhances the Cryopreservation of Cell Monolayers. Biomacromolecules 2019; 20(10): 3864–3872.
13. Pereira J, Ferraretto X, Patrat C, Meddahi-Pellé A. Dextran-Based Hydrogel as a New Tool for BALB/c 3T3 Cell Cryopreservation Without Dimethyl Sulfoxide. Biopreserv. Biobank. 2019; 17(1): 2–10.
14. Wang J, Zhao G, Zhang Z, et al. Magnetic induction heating of superparamagnetic nanoparticles during rewarming augments the recovery of hUCM-MSCs cryopreserved by vitrification. Acta Biomater. 2016; 33: 264–274.
15. Manuchehrabadi N, Gao Z, Zhang J, et al. Improved tissue cryopreservation using inductive heating of magnetic nanoparticles. Sci. Transl. Med. 2017; 9(379): eaah4586.
16. Gao H, Liu Y, Ding J, et al. A Nucleic Acid Quality Control Strategy for Frozen Tissues from a Biobank of High-Risk Pregnancy. Biopreserv. Biobank. 2019; 17: 18–26.
17. Zhang X, Han QY, Zhao ZS, et al. Biobanking of Fresh-Frozen Gastric Cancer Tissues: Impact of Long-Term Storage and Clinicopathological Variables on RNA Quality. Biopreserv Biobank. 2019; 17(1): 58–63.
18. Smith T, Stephan S, Moffett H. et al. In situ programming of leukaemia-specific T cells using synthetic DNA nanocarriers. Nat. Nanotechnol. 2017; 12: 813–820.
19. Tay A. Nonviral Genetic Engineering of CAR T Cells. GEN June 25, 2020.
20. Tay A. Remote Control of CAR T Cells to Enhance Safety. GEN August 5, 2020.
21. He A, Powell S, Kyle M, et al. Cryopreservation of Viable Human Tissues: Renewable Resource for Viable Tissue, Cell Lines, and Organoid Development. Biopreserv. Biobank. 2020; 18(3): 222–227.

