Scientists from Stanley Manne Children’s Research Institute at Ann & Robert H. Lurie Children’s Hospital of Chicago and Northwestern University report they have succeeded in regenerating fully functional urinary bladder tissue in a long-term study utilizing a nonhuman primate model. Their research paves a way for patients with severe bladder dysfunction and has the potential for translation to clinical practice.
Their findings were published in the Proceedings of the National Academy of Sciences (PNAS) Nexus in an article titled, “Multipotent bone marrow cell-seeded polymeric composites drive long-term, definitive urinary bladder tissue regeneration.”
“To date, there are no efficacious translational solutions for end-stage urinary bladder dysfunction,” the researchers wrote. “Current surgical strategies including urinary diversion and bladder augmentation enterocystoplasty (BAE) utilize autologous intestinal segments (e.g., ileum) to increase bladder capacity to protect renal function. Considered the standard of care, BAE is fraught with numerous short- and long-term clinical complications.”
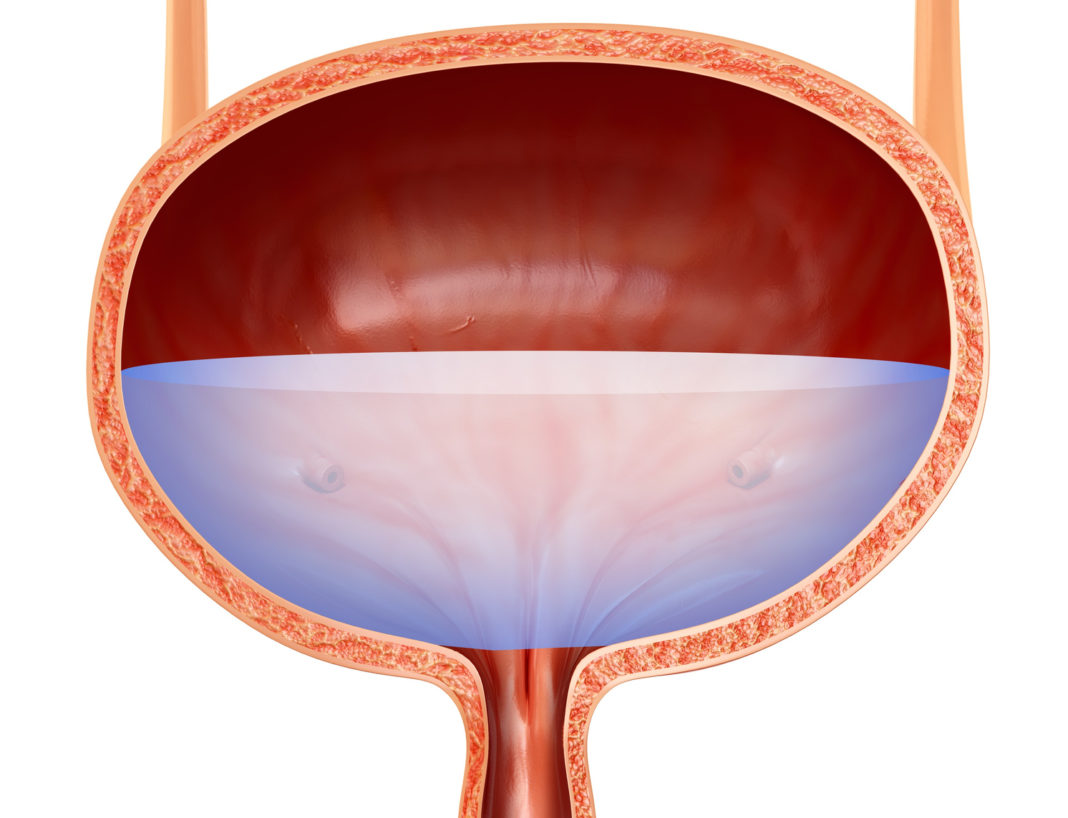
The researchers used a novel biodegradable scaffold seeded with stem and progenitor cells from the animal’s own bone marrow, which demonstrated a higher degree of success than intestinal segments that are traditionally used to treat different types of bladder dysfunction. The regenerated bladder tissue was healthy after two years of monitoring and serves as a preclinical model for humans.
“Our results were fantastic and point to a new direction in the field,” said senior author Arun Sharma, PhD, director of pediatric urological regenerative medicine at Manne Research Institute at Lurie Children’s and research associate professor of urology at Northwestern University Feinberg School of Medicine. “The likelihood that our innovative platform will be feasible in humans is very high and we anticipate launching a clinical trial soon.”
Patients with severe bladder dysfunction have very limited options for bladder tissue replacement. Sharma and colleagues are targeting the pediatric spina bifida population with their bladder regeneration work. Their focus is to offer a better alternative to current bladder augmentation surgery for severe bladder disease. Currently, small intestine tissue is used to replace dysfunctional bladder tissue, but that increases the risk of numerous clinical complications.
“Our innovative approach is promising to make a great difference in the lives of children with spina bifida and others with end stage bladder dysfunction,” said Sharma. “Since we would be using the patient’s own bone marrow cells, there are no concerns with rejection and our scaffold is nontoxic and biodegradable. In our study, the bladder started working within a few months and demonstrated functionality throughout the course of the study. This is a major advance that will transform clinical practice.”