Too often, preclinical successes are followed by clinical failures. And all clinical failures hurt. Perhaps the most painful failures occur in trials that require large patient populations and long treatment periods, such as the trials that have been organized to evaluate therapies for Alzheimer’s disease or nonalcoholic steatohepatitis.
Although time and money are at stake when therapeutic candidates try to cross the preclinical/clinical chasm, other kinds of losses may be incurred. Attention lavished on what appeared to be a promising therapy will, necessarily, be withheld from alternatives—alternatives that may have enjoyed clinical success, alternatives that may have brought relief to those suffering from terrible diseases.
Rather than accept that a yawning preclinical/clinical chasm is an unavoidable fact of life, it might be better to narrow the chasm as much as possible. Then, we could develop therapeutics without having to take breathtaking leaps of faith.
To help make life sciences research and drug development more of a hop, skip, and jump, animal model providers are working to improve the translatability of preclinical results. Essentially, the providers are narrowing the differences between animal models and human patients. They are finding new ways to humanize their animal models more completely.
In this article, humanization initiatives will be described by animal model experts. They will discuss how their work is relevant to a range of disease states, from acne to diabetes to cancer, as well as to varied treatment modalities, including immuno-oncology. They will also describe how ongoing initiatives were sustained in parallel with initiatives meant to address the COVID-19 pandemic.
General issues
In general, animal models reflect safety considerations, technological advances, and efforts to contain emerging threats to health, suggests Andrew G. Reaume, PhD, co-founder, president, and CEO of Melior Discovery, a provider of in vivo pharmacology services. He adds that his company has experience developing models that address each of these considerations.
“Our acne model of sebum production,” he says, “has been significantly improved and validated with isotretinoin.” At present, isotretinoin (Accutane) is one of the only effective acne therapeutics. It is, however, a teratogen that can cause birth defects if it reaches a developing fetus. More than half of all subjects taking the medication are of child-bearing potential and must undergo rigorous birth control programs. Melior’s sebum production mouse model can be used to identify alternative compounds that can reduce sebum production and treat acne more safely than isotretinoin.
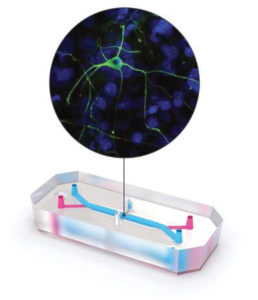
Technological advances of particular interest to Melior concern phenotypic screening. For example, the company has developed theraTRACE, a phenotypic screening tool for drug repositioning, drug repurposing, and indications discovery. (The base platform comprises 40 animal models.) The company has also developed opioidTRACE, an in vivo pharmacology platform for identifying analgesic alternatives to opioids, or opioids with reduced liability.
“Our most notable new models serve pulmonary edema and influenza,” Reaume continues. “Both model a major component of the COVID-19 disease state, namely, the pulmonary barrier leakiness that develops in response to a cytokine storm.”
Refining models
In the pandemic’s early days, the available animal models, such as the LVG Golden Syrian Hamster, were shown to be susceptible to viral infection. They became useful tools in studies of neutralizing antibodies as well as in studies of infection mechanisms. However, it was found that many of the initial ACE2 mouse transgenic models do not reflect severe disease.
Investigators realized that they needed models that are both susceptible to viral infection and also capable of supporting high levels of viral replication. Other requirements include the emulation of functional human hematopoiesis and the engraftment of epi/endothelial cells capable of expressing human ACE2 and other suitable human receptors. Essentially, there was a need for humanized models to support the study of COVID-19.
Humanized models are also advancing other areas of study. In immuno-oncology, humanized mouse models are being developed that can propagate cell line–derived xenograft (CDX) and patient-derived xenograft (PDX) tumors. In the study of age-related diseases—a priority given the growth in aged populations—humanized models are helping investigators avoid having to wait for animals to age naturally.
“Charles River recently introduced the HuCD34-NCG model, a humanized immunodeficient mouse for immuno-oncology studies and infectious disease research, and the C57BL/6 model, an aged mouse for aging research,” says Steve Festin, PhD, director of scientific and commercial development, Research Models and Services, Charles River Laboratories. “The aged C57 mice are animals housed over periods greater than 18 months for studies of animals across different ages produced in a dedicated colony environment.”
Animal models also will become critical in the development of cell- and gene-based therapeutics. To speed the creation of these models, efficient and readily accessible gene modification techniques are needed.
“I find it incredible that, despite a global pandemic, animal models are not in short supply,” Festin asserts. “Our dedicated workers are ensuring that not only industry-standard models are ready, but also that new model projects continue to emerge during the lockdown.”
Ongoing creation
At the Jackson Laboratory (JAX), the Model Generation Service helps to create genetically engineered mouse models to advance the study of cancer, heart disease, diabetes, and neurological disorders, especially Alzheimer’s. JAX also sustains an effort called the Genetic Diversity Initiative, which contains mouse strains and populations featuring stable, well-characterized, segregated genetic variations. These strains and populations are designed to accurately reflect the genetic structure of human populations in many disease areas, improving relevance during therapeutic development.
JAX helps researchers address novel, acute health challenges. For example, when the Zika crisis emerged, JAX rapidly mobilized mouse strains required by researchers, such as Ifnar1 KO mice.
The organization’s response to the COVID-19 pandemic was the first readily available mouse model, the B6.Cg-Tg(K18-ACE2)2Prlmn/J model, which was donated by Stanley Perlman MD, PhD, and Paul McCray, MD, of the University of Iowa Carver College of Medicine. A large distribution colony was quickly generated using advanced reproductive science techniques. Additional COVID-19-related models have been developed, and more are in the queue.
As of last year, over 500 new mouse lines were already available to address various disease and therapeutic areas, such as the MSNASH/PcoJ model, a model for studying obesity, metabolic syndrome, and diabetes in the presumed presence of an intact leptin pathway. Aged colonies for these therapeutic areas were also extended to 90 weeks for B6J males and females, and aged NSG models are readily available.
“In many instances, researchers that access our mouse models may also access our study design and execution services,” says Stephanie Dion, director, JMCRS Business Units, JAX. “This became especially relevant during the pandemic as many stay-at-home orders prevented researchers from performing studies in their own laboratories.
“As treatments become more personalized to the individual and the disease, more attention will be focused on specialty models and their ability to represent the human population. Model complexity will increase, and strain backgrounds will become more diverse. For example, models will harbor larger numbers of genetically engineered alleles, many conditional in nature, to provide a ‘humanized’ physiological environment.”
Addressing complexity
Sophisticated animal models are needed to study diseases that reflect both genetic and environmental factors. Such diseases include cancer, heart disease, diabetes, and neurodegenerative disease, as well as neuropsychiatric disorders involving behavioral complexities that are difficult to proxy in a mouse.
“As we gradually learn more about the genetics of neuropsychiatric disorders that provide a risk status, we can start to develop relevant genetically engineered models,” says Terina Martinez, PhD, field application scientist, Taconic Biosciences. “This is one area where investigators are looking for innovation.”
In response to the COVID-19 pandemic, Taconic launched the AC70 mouse model, originally developed by Chien-Te (Kent) Tseng, PhD, and colleagues at the University of Texas Medical Branch at Houston. The model ubiquitously expresses the human ACE2 receptor that is bound by SARS-CoV-2 spike proteins during viral entry into host cells. Consequently, the AC70 mice respond to clinically relevant viral isolates with translatable effects.
“SARS-CoV-1 research was one of the reasons COVID-19 vaccines got to the clinic quickly,” notes Martinez. “To prepare for the next infectious disease pandemic, models could be deployed faster if exclusive suites were available for different viruses. Different families of viruses have unique, conserved tendencies.”
For applications that require models that have components of the human immune system, Taconic expanded its existing humanized immune system model portfolio with the introduction of the B2m-NOG mouse. The model is based on the super-immunocompromised NOG model originally developed by the Central Institute for Experimental Animals in Japan.
Knocking out beta-2-microglobulin (B2m), part of major histocompatibility complex I, alleviates graft-versus-host disease. Multiple other mutations make the mouse immune system nonfunctional and thus a good receptor for human immune system engraftment. B2m-NOG can accelerate immunological research and immuno-oncology and autoimmune disease studies. In other Taconic NOG models, murine B2m remains intact, and human cytokine genes are inserted to support the reconstitution and function of specific human immune cell subsets.
Martinez believes that progress in precision medicine will require preclinical models that satisfy higher standards for model validation. For example, the antisense oligonucleotides that hold so much promise for treating rare diseases require specialized preclinical models for development and screening.
Fully humanizing antibodies
“We focus on genetically engineered mouse models (GEMMs) for target identification, antibody development, validation, efficacy, and toxicity studies,” says Qingcong Lin, PhD, senior vice president of Biocytogen and CEO of Biocytogen Boston. “We have a lot of IO target knockout/knockin humanized mouse models for immune checkpoint antibody efficacy evaluation, including PD1, PD-L1, Lag3, Tim3, 4-1BB, CD40, and OX40.
“Murine cytokines prevent the survival of some human immune cell subpopulations, so we continually improve our immune humanized models. In the second-generation immunodeficient mouse models, human cytokines or cytokine receptors are knocked in in situ to better support reconstitution of human immune cell subpopulations.” Human cytokine modules can have multiple units (α, β, and γ) that present challenges. Several alterations may be needed to build up the signaling to the cytokine receptor.
Biocytogen’s RenMab mouse is a fully human antibody transgenic mouse whose entire variable regions are replaced by human immunoglobulin heavy chain and κ light chain through a unique megabase-scale chromosome-engineering technology. RenMab antibodies exhibit human-like features as characterized by CDR3 length and VDJ recombination pattern. According to Lin, fully humanized antibodies “allow faster antibody development.”
“With RenMab, we can also knockout antibody targets sequentially to make the immune response stronger, especially for highly homologous, difficult targets, such as G protein–coupled receptors,” Lin adds. “These mice exhibit a robust immune response and provide many hits. We are pursuing industry partnerships to demonstrate these libraries’ usefulness for antibody discovery and screening.”
The RenLite mouse expands the platform with complete humanization in the variable region of the heavy chains, while maintaining a fully humanized common single light chain strategically engineered into the antibody gene for faster bispecific therapeutic antibody discovery.
The RenNano model is scheduled to become available this year. RenNano produces antibodies without heavy chain–light chain pairing, as well as nanobodies. It can support many applications, including antibody-drug conjugate, CAR T-cell, bispecific antibody, and multivalent antibody discovery. Because nanobodies are better able to penetrate the blood-brain barrier, they are especially important in neuroscience. Additionally, the company offers CD3, CD3E, and CD3EDG humanized mice models that support CD3-based antibody discovery programs.
Focusing on oncology
To facilitate the development of next-generation drugs or combination treatments for hard-to-treat cancers, CrownBio is continuing to expand its PDX library. The company is adding models that have been through newer targeted therapies and immuno-oncology treatments and have resulted in either refractory or nonresponsive tumors.
“The next generation of humanized mice needs to have a better reconstitution of the human immune system for use of the PDX system,” says Davy Ouyang, PhD, vice president, scientific research and innovation, CrownBio. “We are working on models to allow development of natural killer cells and myeloid components. In addition, since licensing issues preclude the use of many GEMMs in industry settings, we are rebuilding many models.”
Recently, CrownBio developed 170 new PDX models and 35 CDX and syngeneic imaging-enabled models. The company is also expanding two sister platforms, HuCELL and HuGEMM. HuCELL contains mouse tumor cells engineered to express humanized targets such as PD-L1. HuGEMM contains immunocompetent chimeric mouse models engineered to express humanized drug targets such as genes encoding for immune checkpoint proteins.
“When the target is on the tumor cell, we make a syngeneic tumor line with a humanization of the target,” explains Ouyang. Syngeneic mice retain intact immune systems. Consequently, these mice are particularly relevant for immunotherapy studies. Engineered syngeneic models are made with cells from spontaneous tumors that arise from GEMMs, a mouse version of a PDX model. These cells are transplanted into immunocompetent recipient mice of the same genetic background to test human oncology drugs.
According to Ouyang, animal studies can take advantage of new ways to support the 3Rs—replacement, reduction, and refinement. To address replacement and reduction, CrownBio is expanding its selection of in vitro organoid model systems. (These systems are being developed using the Hubrecht Organoid Technology protocols. Also, CrownBio is converting PDX lines into organoids to offer complementary in vivo and in vitro systems.) To address refinement, CrownBio is deeply profiling models to clarify their most suitable applications.