Drug development is rarely trivial. In fact, it is often costly, frustrating, and tortuous—and more often than not it ends in failure. The sheer complexity of the cell and the astonishing diversity of diseases are just two reasons why researchers typically require years to uncover the mechanisms of disease before they can even dare to contemplate the development of therapeutic options and begin the long, arduous road to the clinic.
Drugs that do make it to clinical trials have major hurdles to clear—not the least of which is safety testing. It is necessary for drugs to evaluated for potential toxicities and side effects, and these key factors must be deemed tolerable before investigators can assess drug potency. For example, chemotherapy, a powerful standard approach to kill fast-growing cancer cells, has the drawback of causing damage to healthy cells in the process, leading to side effects that can include pain, nausea, and hair loss.
Nevertheless, researchers have a host of new technologies at their disposal to develop targeted therapies that minimize side effects. Modern drug development approaches include a range of techniques leveraging structural biology, immunology, cell signaling, and more to address the challenge. As this article shows, progress is being made on multiple fronts.
Targeting interactions rather than individual proteins
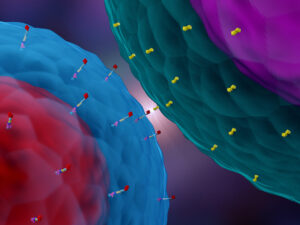
Blue Therapeutics, an IND-stage drug discovery and development platform, addresses the challenges of drug side effects by targeting receptor interactions rather than individual receptors—a concept the company terms the innate proximity paradigm.
Ajay Yekkirala, PhD, chief scientific officer and director of Blue Therapeutics, presented his firm’s latest work at the Cambridge Healthtech Institute’s Discovery on Target conference last September. He elaborates on his firm’s work here, underscoring the limitations of targeting individual receptors only.
Take, for example, the opioid system and the µ-opioid receptor known to regulate pain. “You can make the most selective ligand for µ-opioid receptors if you want to modulate the function of the spinal cord, hypothalamus, and a couple of other areas,” Yekkirala says. “Unfortunately, the receptor is also present in the brainstem and in the opioidergic neurons that project to the limbic system.”
Targeting the µ-opioid receptor could also lead to side effects such as respiratory depression and illustrates a tissue distribution problem. “If we can understand and target the innate proximity of a given interaction, we can spare the activity of the individual receptors, thereby minimizing harmful side effects,” Yekkirala asserts.
The Blue Therapeutics workflow involves identifying receptor interactions that are clearly linked to disease, and then understanding their 3D context by using structural biology techniques such as cryo-electron microscopy (cryo-EM). The next step is to analyze the effect of mutations on these interactions. A great example, Yekkirala notes, is leucine-rich repeat kinase 2 (LRRK2) homo-dimerization, a protein interaction involved in Parkinson’s disease. Mutations in the LRRK2 gene can enhance LRRK2 dimerization and overall kinase function, which then leads to the effects of Parkinson’s.
“Targeting receptor interactions varies case by case, and the complexity goes up because of that,” Yekkirala explains. “At the same time, you’re modulating these interactions, whether [you are] disrupting or enhancing the function. In the end, the tools do come down to simple principles, but now [you are no longer] working with a single receptor, but rather with the full interaction.”
Yekkirala envisions a big future for Blue Therapeutics. Given that the innate proximity approach is dependent on structural biology, Yekkirala states that the rapidly developing tools in protein structure determination and prediction position Blue Therapeutics well to make great strides in neuroscience drug discovery going forward.
Enhancing the body’s own defense system
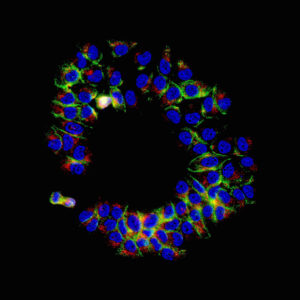
Instead of targeting protein interactions, Kite Pharma, the Los Angeles–based immunotherapy company that was acquired by Gilead Sciences in 2017, seeks to enhance the body’s own immune system. Specially altered T cells can treat cancer through chimeric antigen receptor (CAR) T-cell therapy. In CAR T-cell therapy, T cells are engineered to produce CARs, which enhance the immune system by allowing T cells to latch onto a specific antigen on tumor cells to elicit the immune response.
The big question, Bot says, is this: “Can we actually harness immune cells to be able to eliminate the cancer down to the last cell, in both preventing metastasis and disease recurrence?”
There are two general processes for engineering T cells: autologous, which uses the patient’s own cells, and allogeneic, which uses other cells that can be scalable, such as a third-party donor or induced pluripotent stem cells (iPSCs).
“The autologous process of making cells from each patient is lengthy and more expensive,” Bot observes. He also recognizes that the autologous process can bring engineered T cells to relatively few patients. He is optimistic, however, that the allogeneic process can bring engineered T cells to more and more patients.
“To globally scale up [the production of engineered T cells],” he stresses, “we need a more cost-effective manufacturing process.” That’s where the allogeneic process comes into play. “The cost of goods would be significantly lower,” Bot asserts. “For example, you can create 10,000 batches from a cell population derived from pluripotent stem cells.”
Despite the advantages of the allogeneic products, the mechanics of how allogeneic cells and autologous cells may work differently is still poorly understood. Data establishing whether allogeneic products recapitulate the potency of autologous products is still awaited.
The role of DNA repair proteins in cancer
Enhancing the immune system is one of many promising approaches toward targeted cancer treatment. How else can an understanding of cell signaling shed light on the mechanisms of cancer? Researchers at Sanford Burnham Prebys, a biomedical research institute based in San Diego, are tackling this question.
In Haricharan’s view, cancer cells exhibit “stressed out” behaviors—such as turning off cell cycle checkpoints (which regulate cell division) and apoptotic pathways (which govern programmed cell death)—to proliferate at a harmful degree. DNA damage repair proteins are instrumental in turning on cell cycle checkpoints in response to therapy.
“[We realized that] 30% percent of these patients have turned off these DNA damage repair proteins and don’t respond to therapy,” Haricharan recalls. “We then asked, ‘Is there a way we can go downstream of the DNA damage repair proteins and turn on the cell cycle checkpoints using drugs?’”
In a recent paper (Punturi et al. Nat. Commun. 2021; 12(1): 2940), Haricharan and colleagues demonstrated the importance of understanding cell signaling. Her team showed that in the absence of DNA damage repair proteins, cells start activating HER2, a crucial growth-promoting protein on the outside of breast cells and a highly druggable target.
“The presence of DNA damage proteins has been routinely diagnosed in the clinic for ages now,” Haricharan notes. “In the past, we didn’t know that this diagnostic was linked to therapeutic action. By understanding the signaling, we now have made this diagnostic meaningful in a therapeutic sense.” Haricharan’s HER2 project is currently moving into clinical trials.
Targeting deregulated cell signaling in breast cancer
Haricharan’s colleague, Brooke Emerling, PhD, assistant professor in the Cell and Molecular Biology of Cancer Program, studies cell signaling in cancer treatment from a different angle. The Emerling laboratory focuses on lipids, key structural components of cell membranes. But Emerling emphasizes that their functionality is quite diverse. In cell signaling, lipids provide a docking platform for proteins to bind and perform key cellular and metabolic processes.
Emerling says that tumor microenvironments are often deprived of nutrients. Cells turn on key metabolic pathways moderated by lipids to withstand these harsh conditions. While normal cells would die, cancer cells have mechanisms that prevent cell death and allow proliferation. Emerling notes that phosphoinositide 3-kinases (PI3Ks) and tumor protein p53 are key lipid signaling proteins known to harbor “hotspot” mutations for cancer growth.
While the work in Emerling’s laboratory is broadly applicable across cancers, it is mainly focused on breast cancer. “A lot of proteins aren’t mutated in cancers—they’re deregulated,” she points out. “In the enzymes that we study, we found that they were highly upregulated in breast cancers.”
“It’s an unmet need where we don’t have targeted therapies for these p53 mutant cancers, particularly triple-negative breast cancer,” Emerling continues.
The well-known tumor suppressor protein p53 is difficult to target directly. To address this challenge, Emerling aims to develop drugs that target signaling enzymes called kinases that are deregulated due to p53 mutations. Emerling explains that drug screens are first performed to determine whether candidates successfully target the enzyme of interest. Successful drug candidates are then taken to the cell biology lab, where experiments are performed on breast cancer cells to evaluate cell viability and other responses to the drug.
“[These drug candidates] are a targeted therapy where you’re not blanketly applying chemotherapy or radiation,” Emerling details. “Instead, we’re targeting enzymes that are specifically turned on during these oncogenic events.”
Both Haricharan and Emerling contribute to drug screening projects of the Conrad Prebys Center for Chemical Genomics. In these projects, Haricharan and Emerling focus on DNA damage repair and lipid signaling, respectively.


