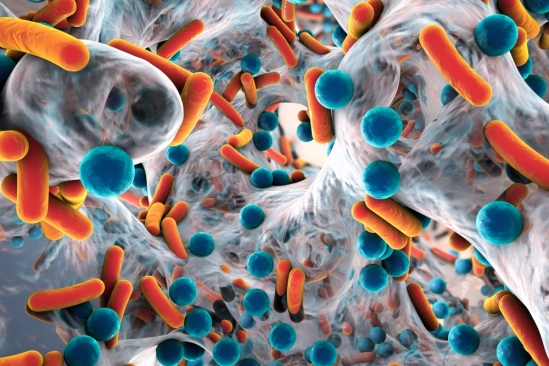
Differences in the composition of gut microbes have been linked to a wide variety of human conditions, from obesity and inflammatory bowel diseases to depression and schizophrenia. The use of some medications, such as stomach acid neutralizers—proton pump inhibitors—are associated with disruption of the microbial communities of the gut. Now, researchers find that statins could potentially modulate the disrupted gut microbiota and linked inflammation in obesity.
The findings are published in Nature in a paper titled, “Statin therapy is associated with lower prevalence of gut microbiota dysbiosis.”
The study of the microbiome has revealed a microbiota configuration, the Bacteroides2 (Bact2) enterotype, to be associated with systemic inflammation and is prevalent in loose stools in humans. Bact2 is characterized by a high proportion of Bacteroides, a low proportion of Faecalibacterium, and low microbial cell densities. The authors of the paper write that “its prevalence varies from 13% in a general population cohort to as high as 78% in patients with inflammatory bowel disease.”
The researchers were from the MetaCardis Investigators, an EU-funded research project investigating the role of gut microbes in cardiometabolic diseases (CMDs) that use metagenomics and the use of clinical and experimental studies.
The team, led by Jeroen Raes, PhD, professor at the laboratory of molecular bacteriology, department of microbiology and immunology, Rega Institute, KU Leuven, Belgium, sought to understand if the changes in stool consistency and inflammation status during the progression towards obesity and metabolic comorbidities might similarly correlate with an increased prevalence of the Bact2 enterotype.
The intestinal microbiota in obese individuals had previously been shown to differ from those in lean subjects with a poor bacterial diversity, a relative depletion of health-promoting bacteria, and the remaining bacteria dominated by an inflammatory tone.
To study this, the group explored gut bacteria in almost 900 individuals from Denmark, France, and Germany. By exploring obesity-associated microbiota alterations in the fecal metagenomes of the cross-sectional MetaCardis Body Mass Index Spectrum cohort, they were able to identify statin therapy as a potential factor of microbiome diversification.
In a group of participants that were not medicated with statins—a group of cholesterol-lowering medications—the team found that the prevalence of Bact2 correlates with body mass index, increasing from 3.90% in lean or overweight participants to 17.73% in obese participants.
However, in other obese study participants who were treated with statins, the prevalence of the unhealthy Bact2 enterotype was significantly lower (6%) than in their non-treated counterparts (18%)—comparable to levels observed in non-obese participants (4%).
This finding was validated in both the accompanying MetaCardis cardiovascular disease dataset (n = 282) and the independent Flemish Gut Flora Project population cohort (n = 2,345).
Statins are commonly prescribed to reduce the risk of developing cardiovascular diseases like myocardial infarction and stroke. It is estimated that more than 200 million people worldwide are prescribed statins. Besides their cholesterol-lowering effects, statins also tend to appease patients’ systemic inflammation levels which in part may be related to disrupted gut microbiota.
The results suggest that statins could potentially modulate the disrupted gut microbiota and linked inflammation in obesity. Previous experiments in rodents have shown an impact of statins on bacterial growth, which might benefit non-inflammatory bacteria and underlie the anti-inflammatory effects of statin therapy.
More work is needed to address whether statins mediate some of their anti-inflammatory effect via an improvement of the Bact2 enterotype of aberrant gut microbiota. The authors noted that the potential benefits of statins in this context “will require further evaluation in a prospective clinical trial to ascertain whether the effect is reproducible in a randomized population and before considering their application as microbiota-modulating therapeutics.”