Electrophoresis-based, functional screening of metabolites produced by resident gut microbiota from patients with inflammatory bowel disease (IBD) showed that generally harmless bacteria (commensals) produce a diverse range of metabolites that can damage DNA (genotoxins). According to the study published in the journal Science these genotoxic metabolites may play a role in the development of colorectal cancer—the second leading cause of global cancer deaths. Individuals with IBD are at increased risk of developing colorectal cancer.
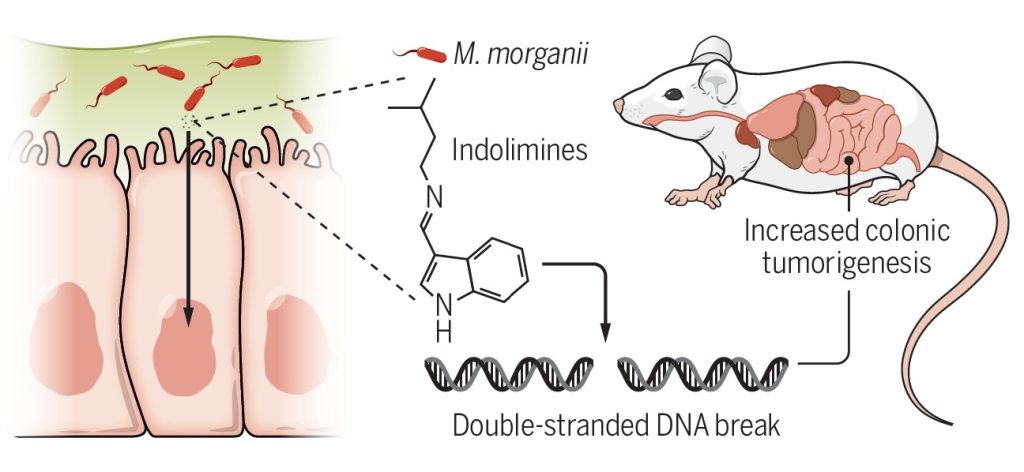
The authors, scientists at the Yale University School of Medicine discovered a family of genotoxins called indolimines, that are produced by Morganella morganii—a bacterial species linked to colorectal cancer. The researchers showed that indolimines can generate double-stranded breaks in DNA, in both cell-free and cell-based DNA damage assays. Such double-strand DNA damage could trigger the development of cancer.
Earlier studies had shown that microbiota-derived genotoxic metabolites likely play a critical role in driving pathogenesis that leads to colorectal cancer, but the identity of the spectrum of genotoxic chemicals produced by commensal gut microbes in IBD was unknown.
In the current study, Yiyun Cao, a graduate student, and her colleagues in the laboratory led by Noah Palm, an associate professor of immunobiology at the Yale school of medicine, combined untargeted metabolomics and bioactivity-guided natural product discovery techniques to isolate and characterize indolimines.
They demonstrated that, in a mouse model of colon cancer, the presence of aat (aspartate aminotransferase) expressing Morganella morganii in the gut microbiota exacerbated tumor growth. However, a non-indolimine-producing mutant strain of the same bacterial species lacked this genotoxicity and did not promote tumor growth. This observation indicates that the production of indolimines is required to promote the growth of tumors in the colon when these bacteria are transplanted into a susceptible mouse model. The researchers have also identified other bacteria belong to the phyla Firmicutes and Actinobacteria that produce metabolites that are likely to be genotoxic.
“These studies reveal the existence of a previously unexplored universe of genotoxic small molecules from the microbiome that may affect host biology in homeostasis and disease,” the authors concluded. These findings can help identify novel genotoxicity mechanisms that trigger disease.