The importance of detecting viral aerosols, and specifically SARS-CoV-2, was brought to the forefront during the COVID-19 pandemic. To date, techniques for the detection of viruses in indoor environments have limitations: long turnaround times and a requirement of skilled labor.
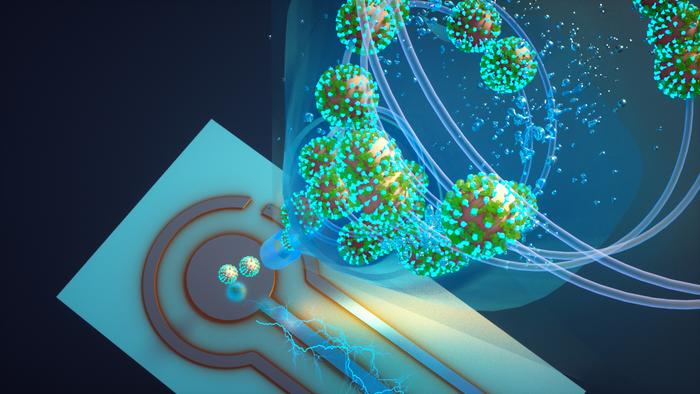
Now, by combining aerosol sampling technology and an ultrasensitive biosensing technique, researchers report the creation of a real-time monitor that can detect SARS-CoV-2 virus (and variants) in a room in about five minutes. The proof-of-concept device could be used in hospitals and health care facilities, schools, and public places to help detect SARS-CoV-2 and potentially monitor for other respiratory virus aerosols, such as influenza and respiratory syncytial virus (RSV).
This work is published in Nature Communications in the paper, “Real-time environmental surveillance of SARS-CoV-2 aerosols.”
“There is nothing at the moment that tells us how safe a room is,” said John Cirrito, PhD, a professor of neurology at the School of Medicine at Washington University, St. Louis. “If you are in a room with 100 people, you don’t want to find out five days later whether you could be sick or not. The idea with this device is that you can know essentially in real time, or every five minutes, if there is a live virus.”
Cirrito and colleagues had previously developed a micro-immunoelectrode (MIE) biosensor that detects amyloid beta as a biomarker for Alzheimer’s disease. They wondered if it could be converted into a detector for SARS-CoV-2. To convert the biosensor from detecting amyloid beta to coronavirus, the researchers exchanged the antibody that recognizes amyloid beta for a nanobody from llamas that recognizes the spike protein from the SARS-CoV-2 virus.
“The nanobody-based electrochemical approach is faster at detecting the virus because it doesn’t need a reagent or a lot of processing steps,” said Carla Yuede, PhD, an associate professor of psychiatry at the School of Medicine. “SARS-CoV-2 binds to the nanobodies on the surface, and we can induce oxidation of tyrosines on the surface of the virus using a technique called square wave voltammetry to get a measurement of the amount of virus in the sample.”
The biosensor was integrated into an air sampler that operates based on wet cyclone technology. Air enters the sampler at very high velocities and gets mixed centrifugally with the fluid that lines the walls of the sampler to create a surface vortex, thereby trapping the virus aerosols. The wet cyclone sampler has an automated pump that collects the fluid and sends it to the biosensor for seamless detection of the virus using electrochemistry.
“The challenge with airborne aerosol detectors is that the level of virus in the indoor air is so diluted that it even pushes toward the limit of detection of polymerase chain reaction (PCR) and is like finding a needle in a haystack,” said Rajan Chakrabarty, PhD, associate professor of energy, environmental & chemical engineering in McKelvey Engineering. “The high virus recovery by the wet cyclone can be attributed to its extremely high flow rate, which allows it to sample a larger volume of air over a five-minute sample collection compared with commercially available samplers.”
The team’s monitor has a flow rate of about 1,000 liters per minute, making it one of the highest flow-rate devices available. It is also compact at about 1 foot wide and 10 inches tall and lights up when a virus is detected, alerting administrators to increase airflow or circulation in the room.
The team tested the monitor in the apartments of two COVID-positive patients. The real-time PCR results of air samples from the bedrooms were compared with air samples collected from a virus-free control room. The devices detected RNA of the virus in the air samples from the bedrooms but did not detect any in the control air samples.
In laboratory experiments that aerosolized SARS-CoV-2 into a room-sized chamber, the wet cyclone and biosensor were able to detect varying levels of airborne virus concentrations after only a few minutes of sampling. More specifically, the experiments demonstrate a device sensitivity of 77–83% and a limit of detection of 7–35 viral RNA copies/m3 of air.
“We are starting with SARS-CoV-2, but there are plans to also measure influenza, RSV, rhinovirus, and other top pathogens that routinely infect people,” Cirrito said. “In a hospital setting, the monitor could be used to measure for staph or strep, which cause all kinds of complications for patients. This could really have a major impact on people’s health.” The team is working to commercialize the air quality monitor.