A study conducted in mice by researchers in the lab of Irvine Weissman, MD, at Stanford University School of Medicine, and at the National Institutes of Health’s Rocky Mountain Laboratories, has provided evidence that it may be possible to rev up an elderly immune system using a one-time antibody treatment that modulates the composition of a type of immune cell.
The results of the team’s research showed that the approach, targeting a subset of hematopoietic stem cells (HSCs) that increase with age, rebalanced blood-cell production and reduced age-related immune decline. The treatment significantly improved the ability of geriatric animals’ immune systems to tackle a new virus, and to respond to vaccination, enabling the animals to fight off a new viral threat months later.
“This is a real paradigm shift—researchers and clinicians should think in a new way about the immune system and aging,” said Stanford postdoctoral scholar Jason Ross, MD, PhD. “The idea that it’s possible to tune the entire immune system of millions of cells simply by affecting the function of such a rare population is surprising and exciting.”
Weissman, who is professor of pathology and of developmental biology, and Kim Hasenkrug, PhD, the chief of Rocky Mountain Laboratories’ Retroviral Immunology Section, are senior authors of the team’s published study in Nature, titled “Depleting myeloid-biased haematopoietic stem cells rejuvenates aged immunity.” Ross and Lara Myers, PhD, a research fellow at Rocky Mountain Laboratories, are lead authors of the report, in which the team concluded, “The clinical development of safe protocols to rebalance HSCs could have broad effects on a number of age-associated issues.”
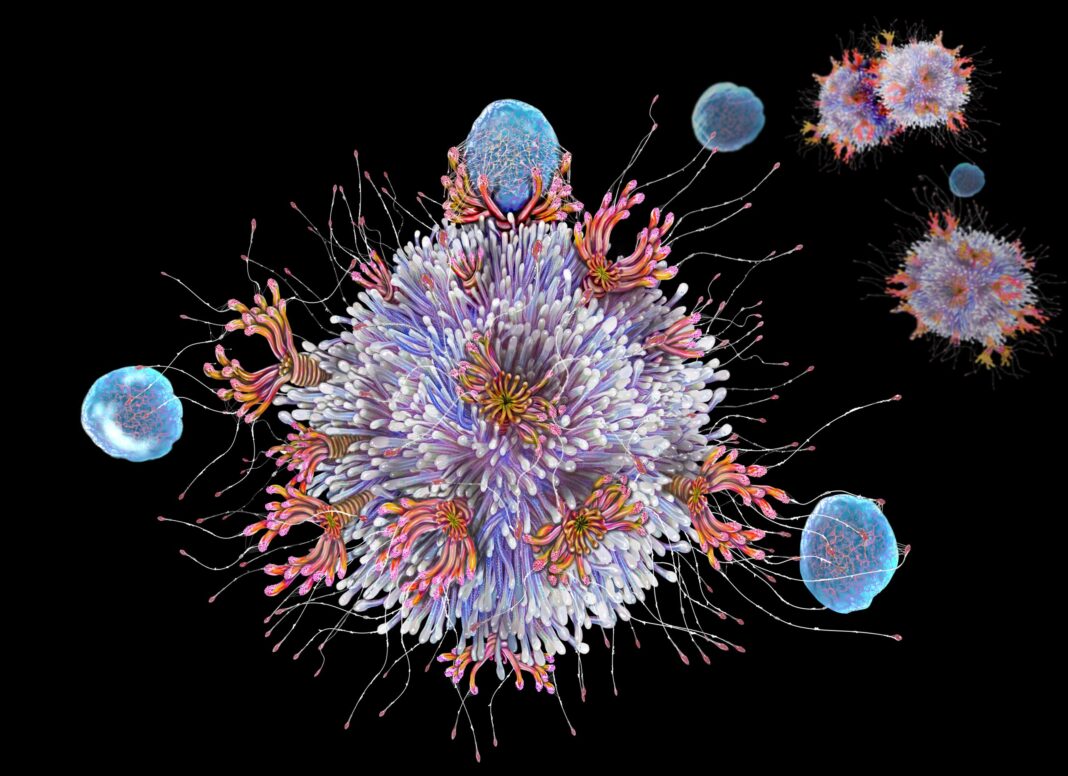
HSCs are immune system progenitors that give rise to all the other types of blood and immune cells including myeloid cells, and B and T lymphocytes. “A single HSC can generate all blood cells and self-renew to maintain the stem cell pool throughout life,” the team wrote. “At least two HSC subsets exist: (1) bal-HSCs, which provide balanced production of lymphoid and myeloid cells; and (2) my-HSCs, which are biased towards predominant production of myeloid cells.”
As we age, our HSCs begin to favor the production of myeloid cells over lymphocytes. This shift hampers our ability to fully react to new viral or bacterial threats, and makes response to vaccination much less robust than that of younger people. “This age-related shift from bal-HSCs to my-HSCs decreases lymphopoiesis and increases myelopoiesis, thereby contributing to numerous pathologies in older individuals, including reduced adaptive immunity, inflammaging and several myeloid-related diseases,” the team further commented.
Weissman, who is the Virginia and D.K. Ludwig Professor in Clinical Investigation in Cancer Research, added, “Older people just don’t make many new B and T cell lymphocytes. During the start of the COVID-19 pandemic it quickly became clear that older people were dying in larger numbers than younger people. This trend continued even after vaccinations became available. If we can revitalize the aging human immune system like we did in mice, it could be lifesaving when the next global pathogen arises.” The team added, “A hallmark of immune aging is reduced resistance to infection and responsiveness to vaccination, as became evident during the COVID-19 pandemic.”
Weissman was the first to isolate HSCs in mice and humans in the late 1980s, and in the years since he and his colleagues have investigated the molecular minutiae of these cells, tracing the complicated relationships among the many different cell types to which they give rise.
Some of these descendants comprises highly specialized B and T lymphocytes that are part of the adaptive immune system. The specificity of B and T lymphocytes allows the immune system to have memory, such that a second exposure to a previously encountered pathogen triggers the body to react swiftly. This is the basic concept behind vaccination— trigger an initial response to a harmless mimic of a dangerous bacteria or virus. In response, the lymphocytes that recognize the invader not only give rise to cells that eliminate the infection but also generate long-lived memory B and T cells that, in some cases, can last a lifetime. This effectively primes the immune system in the event that the threat becomes real.
Another key part of the immune system, innate immunity, is much less discriminating. In the blood, myeloid cells effectively clean up unfamiliar cells or bits of detritus, and also trigger inflammatory responses at infected sites. Inflammation helps the body protect itself against invaders, but it can be a major problem when triggered inappropriately or overenthusiastically, and aging has been linked to chronic inflammation in humans.
Ross and Weissman knew from previous research that during aging, the number of HSCs that make balanced proportions of lymphocytes and myeloid cells decline, while those that are myeloid-biased increase their numbers. This favors the production of myeloid cells.
Early in human history, when people rarely left their birthplace and lived shorter lives, this gradual change probably had no consequences, and may even have been favorable, because people were likely to encounter all their surrounding pathogens by young adulthood and be protected by their memory lymphocytes.
“The evolution of the vertebrate immune system occurred in geographically limited populations,” the authors wrote. “Before machine-mediated transportation— trains, planes, boats and cars—individuals were likely to be exposed to the majority of pathogens in their local geography by the time of reproductive age.” As T and B memory/stem cells can survive an individual’s lifetime, and for such populations they should be sufficient to provide adaptive immune memory to all local pathogens. “Thus, the generation of new T and B lymphocytes in later life was probably no longer advantageous, whereas the production of short-lived myeloid cells would remain important for acute innate responses, even in later life.”
With the advent of global travel, however, this change in HSC pool from bal-HSCs to my-HSCs during aging could be distinctly disadvantageous. “… the introduction of geographical migration by modern transportation created novel exposures of individuals to pathogens first encountered later in life when T and B cells are no longer efficiently produced,” the team continued. “The haematopoietic system shift to myeloid-biased production has probably enabled novel pathogens to cause global pandemics.”
For their reported study Irving Weissman and colleagues aimed to test, in aging mice, whether it was possible to tilt the balance back toward a younger immune system, using an immunotherapy designed to deplete these myeloid-leaning HSCs and allow the more balanced HSCs to replace them. To do this the authors first identified cell surface proteins on the myeloid-biased subset of HSCs, that were not found on the HSCs with balanced output, and which could be targeted by antibodies.
Their preclinical study confirmed that in older mice between 18 and 24 months of age treatment using an antibody that targeted the myeloid-leaning HSCs for destruction had more of the balanced HSCs, and more new, naïve B and T lymphocytes, than their untreated peers, even several weeks later. “The increase in lymphoid progenitors and decrease in myeloid progenitors after my-HSC depletion in adult mice pointed to the potential of this treatment to reverse age-related immune decline,” the investigators stated.
“These new, naïve lymphocytes provide better immune coverage for novel infections like those humans increasingly encounter as our world becomes more global,” Weissman said. “Without this renewal, these new infectious agents would not be recognized by the existing pool of memory lymphocytes.”
The treatment also reduced some negative outcomes like inflammation that can arise when an elderly immune system grapples with a new pathogen. “… in addition to resulting in a more youthful composition of immune cells, my-HSC depletion decreased the levels of circulating pro-inflammatory mediators several months after treatment,” the team reported. “Not only did we see a shift toward cells involved in adaptive immunity, but we also observed a dampening in the levels of inflammatory proteins in the treated animals,” Ross said. “We were surprised that a single course of treatment had such a long-lasting effect. The difference between the treated and untreated animals remained dramatic even two months later.”
When the treated animals were vaccinated eight weeks later against a virus they hadn’t encountered before, their immune systems responded more vigorously than those of untreated animals, and the treated mice were significantly better able to resist infection by that virus. “Depletion of my-HSCs in aged mice improves primary and secondary adaptive immune responses to viral infection,” the team stated. In contrast, young mice used as controls passed all the challenges without issue.
“Here we demonstrate that antibody-mediated depletion of my-HSCs in aged mice restores characteristic features of a more youthful immune system, including increasing common lymphocyte progenitors, naive T cells and B cells, while decreasing age-related markers of immune decline,” the authors summarized in their report. “Every feature of an aging immune system—functional markers on the cells, the prevalence of inflammatory proteins, the response to vaccination and the ability to resist a lethal infection—was impacted by this single course of treatment targeting just one cell type,” Ross said.
Finally, the researchers showed that mouse and human myeloid-biased HSCs are similar enough that it may one day be possible to use a similar technique to revitalize aging human immune systems, perhaps making a person less vulnerable to novel infections and improving their response to vaccination. “… all three mouse my-HSC markers that we demonstrated as therapeutic targets for my-HSC depletion in vivo—CD150, CD62p and NEO1—were also present on the cell surface of a subset of human HSCs,” the authors commented. “The conservation between mouse and humans of the expansion of my-HSCs and of the genes that increase during HSC aging suggests that this preclinical study could support the development of clinical therapies to rejuvenate the blood-forming system in patients.”
Ross noted, “We believe that this study represents the first steps in applying this strategy in humans.” The authors acknowledged the need for additional studies. “Further research will be required to optimize conditioning protocols, possibly using combinations of antibodies against my-HSC-specific markers while considering possible effects on differentiated cells such as regulatory T cells,” they wrote.
The work also has interesting implications for stem cell biology and the way HSCs rely on biological niches, or specific neighborhoods of cells, for their longevity and function throughout our lives. “Most people in immunology have believed that you lose these kinds of tissue-specific stem cells as you grow older,” Weissman said. “But that is completely wrong. The problems arise when you start to favor one type of HSC over another. And we’ve shown in mice that this can be reversed. This finding changes how we think about stem cells during every stage of aging.”
Writing in their paper, the investigators further noted that their findings could feasibly have applications in a range of therapeutic areas. “Rejuvenating the immune system with bal-HSCs could also restore the surveillance systems required for elimination of transformed and partially transformed cells that drive cancer, and/or reduce the generation of myeloid cells that suppress tumour immunity. Such an approach could support both T-cell-based and myeloid-based immunotherapies, or reverse the inflammation and/or depletion of cells that result from cytotoxic anti-cancer therapies including chemotherapy and radiotherapy. Our study provides proof-of-principle for translational studies focused on applying similar strategies to improve functional immunity combat infections, chronic disease and cancer.”