Researchers headed by a team at Queen Mary University of London have discovered that melanoma cells can survive anti-cancer immunotherapy by altering their cytoskeleton. The scientists’ laboratory studies in patient-derived cancer cells and experiments in live mice showed that melanoma cells stopped responding to immunotherapies and drugs targeting commonly mutated MAPK pathway genes BRAF or NRas by increasing the activity of two cytoskeletal proteins, ROCK and myosin II. These two proteins were found to be key to cancer cell survival and resistance to these treatments.
The results point to a strong connection between metastasis and therapy resistance, and the importance of the cytoskeleton in determining the aggressiveness of cancer. The findings could feasibly help researchers develop new therapeutic approaches against skin cancer and other tumor types that develop resistance to treatment. Victoria Sanz-Moreno, PhD, Professor of Cancer Cell Biology at Queen Mary, said, “We were very surprised to find that the cancerous cells used the same mechanism, changing their cytoskeleton, to escape two very different types of drugs. In a nutshell if you are a cancer cell, what does not kill you makes you stronger. However, their dependence on ROCK-myosin II is a vulnerability that combination drug therapy tests on mice suggest we can exploit in the clinic by combining existing anti-melanoma therapies with ROCK-myosin II inhibitors.”
Sanz-Moreno and colleagues report their findings in Cancer Cell, in a paper titled, “Myosin II Reactivation and Cytoskeletal Remodeling as a Hallmark and a Vulnerability in Melanoma Therapy Resistance.”
Malignant melanoma has very poor survival rates even though it is at the forefront of personalised immunotherapy, the authors explained. Around 16,000 people in the UK are diagnosed with malignant melanoma each year, and the disease causes more than 2,300 deaths. “Despite substantial clinical benefit of targeted and immune checkpoint blockade-based therapies in melanoma, resistance inevitably develops,” the researchers wrote. The BRAF V600 mutation represents the most common oncogene in melanoma, and promotes cancer cell proliferation, survival, and tumor progression, by hyperactivating MEK and ERK kinases. However, targeted BRAF inhibitors (BRAFi) haven’t had great success in the clinic, as the disease progresses in most patients due to acquired resistance. “Often, patients with resistance develop more metastases and 20% of BRAF mutant melanoma patients never respond to BRAFi due to intrinsic resistance,” the team continued.
Most resistance mechanisms involve MAPK reactivation, but treated patients will commonly relapse even when treated using a combination of BRAF inhibition and an MEK inhibitor (MEKi). And while improved survival has been demonsrated in melanoma patients treated using immune checkpoint inhibition (anti-PD-1 and anti-CTLA-4), again, patients commonly do not respond or relapse due to resistance.
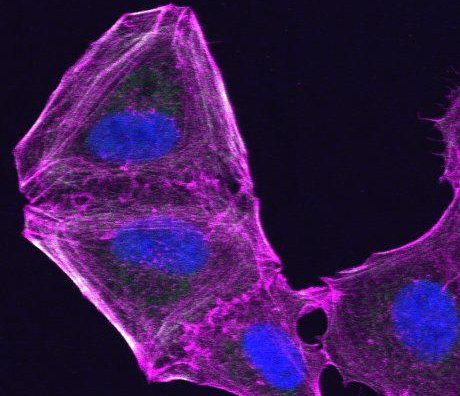
A better understanding of the biological/biochemical changes in resistant cells will help scientists develop improved treatments, the authors stated. What has been observed is an overlap between cancer cell migration and pro-survival pathways, and drivers of resistance have been linked to metastatic ability. Interestingly, the ROCK-myosin II pathway is already known represent a key regulator of invasive and metastatic behaviour. However, while the two molecules had previously been linked to the process of metastatic spread, it wasn’t known whether there was also a link between this pathway and poor response to current anti-melanoma therapies. “Given the activation of pro-invasive/metastasis pathways during melanoma cross-resistance, we sought to investigate the role of cytoskeletal remodeling in therapy resistance,” the authors wrote.
Their laboratory tests on cells in culture confirmed that melanoma cells can adapt to therapy by “rewiring their transcriptome” to change cytoskeletal gene expression and restore myosin II activity, which is key for melanoma surviving treatment. The in vitro experiments also confirmed that survival of targeted therapy-resistant melanomas is dependent on ROCK-driven myosin II activity. “… myosin II restoration confers a survival advantage to resistant melanoma,” they wrote. Interestingly an analysis of data on human melanoma samples showed that higher ROCK-myosin II in treatment-naïve melanoma patients was associated with worse prognosis. “We suggest that melanomas with intrinsically higher expression of the ROCK-myosin II pathway are more aggressive and prone to develop resistance,” they commented. Further tests using melanoma cells from patient samples confirmed that “melanomas with acquired and primary resistance to targeted and immunotherapies rely on myosin II activity for their survival.”
The team was interested to know why resistant cells relied on myosin II for survival. Further tests showed that resistant melanoma cells had high levels of oxidative stress and reactive oxygen species (ROS) metabolism gene signatures. Blocking myosin II activity effectively overcame treatment resistance in melanoma by introducing lethal ROS, unresolved DNA damage, and loss of pro-survival signaling, which leads to cell-cycle arrest and cell death.
In vivo experiments in mice further supported the notion that therapy-resistant (or non-responding) tumours required ROCK-myosin II to grow. The team’s studies in the animals demonstrated that BRAFi and ROCKi inhibitor combination therapy shrank BRAFi-resistant tumors and improved mouse survival. A combination of ROCK-myosin II inhibition and anti-PD-1 inhibition also led to significantly increased regression of established tumors than did either treatment alone. The results in addition indicted that ROCK-myosin II inhibition attacks faulty macrophages and regulatory T cells that fail to kill the tumour. “… blocking ROCK-myosin II reduces immunosuppressive microenvironments, improving anti-PD-1 action on pre-existing T cells,” the team noted.
First author, Jose L. Orgaz, PhD, Research Fellow at Queen Mary’s Barts Cancer Institute, commented, “An important observation was finding increased myosin II activity levels in resistant human melanomas, which suggests the potential as a biomarker of therapy failure. Resistant melanomas also had increased numbers of faulty immune cells (macrophages and regulatory T cells), which could also contribute to the lack of response.”
“In summary, we provide extensive evidence that targeting cytoskeletal regulators Driving high myosin II activity overcomes resistance to targeted and immunotherapies in Melanoma,” the scientists stated. They suggest that the findings point to the possibility that cytoskeletal remodeling may represent “a conserved pro-survival mechanism of generating therapy resistant cancer clones under the selection of other therapy regimes.” And while such cytoskeletal adaptations that occur very early on treatment provide the tumor cells with a survival advantage, they also represent “ …. a vulnerability, which can be later exploited.”
Rock inhibitors (ROCKi) have been used since the 1990s to treat subarachnoid haemorrhage, and are also used as vasodilators to lower blood pressure. Candidates are now being evaluated in clinical trials for vascular diseases including glaucoma, pulmonary hypertension and atherosclerosis, the authors pointed out. The newly reported results indicate that ROCKi candidates could also be evaluated in cancer therapy. “Optimal ROCKi could be tested in broader range of disease, as a strategy to extend clinical response to different cancer therapies or even as a single therapy in the case of drug-addicted tumors … Importantly, therapy-resistant cells are more sensitive to ROCKi while its combination with current therapies seems to elicit a superior response.”