During the COVID-19 pandemic, mRNA-based vaccines led the charge against the SARS-CoV-2 virus. These therapies would not have existed were it not for the painstaking mRNA research that began years before the pandemic. The lesson? It is important to be prepared. Let us remember that always, for we are bound to see more pandemics in the future.
More generally, we make a virtue of preparedness in all of our healthcare efforts. As the researchers interviewed here would no doubt agree, many of these efforts could benefit from applications of mRNA technology. The recently introduced mRNA-based vaccines represent just the start of what mRNA technologies can—and will—achieve.
Making ends meet
More than a decade ago, while spending a year working in a laboratory before entering medical school, a budding scientist got interested in circular mRNA, which (unlike linear mRNA) is in the form of a continuous, covalently closed loop. Today, that scientist—Robert Kruse, MD, PhD, clinical fellow, Harvard Medical School—recalls that he was “thinking about mRNA as a therapeutic and how to improve the properties.” He wondered whether circular mRNA could outperform linear mRNA or even do things that linear mRNA couldn’t.

Back then, no one knew if circular mRNA could even be translated inside a human cell. Kruse, however, showed that it was possible. (He did so while he was pursuing a medical degree and a doctorate in translational biology and molecular medicine at Baylor College of Medicine.) His work led to an early patent in the circular mRNA field.
But can circular RNA be made at scale as a drug? That turns out to be possible, too. In a test tube, autocatalytic, intron-splicing RNA from bacteriophages can yield “mRNA that will self-catalyze and create a circle by itself,” Kruse explains.
The process was refined by a graduate student at the Massachusetts Institute of Technology. Indeed, that student—who is now better known as R. Alexander Wesselhoeft, PhD, founder and director of molecular biology at Orna Therapeutics—made the process efficient enough that most of the mRNA made in test tube reactions turns into circles that can then be used for vaccines or therapies.
Kruse observes that there is significant interest in circular mRNA for therapies. Some companies focused on circular mRNA—such as Orna Therapeutics and Laronde—are garnering sizable investment rounds. As he explains, circular mRNA is a promising therapeutic modality because the molecule’s half-life is “three to four times longer” than linear mRNA’s half-life. Consequently, circular mRNA gets expressed far longer.
An extended half-life could improve the use of mRNA in various applications. In vaccines, for example, a lower dose of circular mRNA might provide the same efficacy as a higher dose of linear mRNA, which could reduce the cost and potential side effects. Similarly, cancer therapies based on circular mRNA could allow less frequent treatments.
“Instead of giving linear mRNA to cancer patients every week, maybe circular mRNA could be given only twice a month,” Kruse suggests. “That would be more convenient for patients, and it could be a lot less toxic for them.”
Still, Kruse notes that some of these applications remain theoretical. Although mouse studies show high levels of expression from circular mRNA, the same remains to be shown in humans. In addition, the tolerability of chronic dosing of mRNA therapeutics in humans also remains unknown. For both issues, Kruse says, “Scientists need to figure this out over time.”
Making more mRNA
Besides increasing the expression of a desired protein, perhaps by using circular mRNA instead of linear RNA, it is possible to increase the level of a desired mRNA. One may simply increase the mRNA dose, or one may use a different kind of RNA, namely, self-amplifying mRNA (sa-mRNA). The second option has been researched for a number of years by scientists at Seqirus.

Vice President, Research Seqirus
“In the case of sa-mRNA, the RNA goes into the cell, and there’s an extra element on the mRNA molecule—replicase—that allows the RNA to replicate itself,” says Ethan Settembre, PhD, vice president of research for Seqirus. “Each of those RNA copies creates the protein of interest.” So, the replication of mRNA makes more protein to generate an immune response.
The replicase comes from alphavirus. As Settembre says, “I often like to work with nature, rather than against it.” In this application, nature’s solution can increase the level of the mRNA so much that protein expression increases 80- to 100-fold, compared to using ordinary mRNA.
As a result, an sa-mRNA-based vaccine or therapy could be given at a lower dose and still achieve the same efficacy as an mRNA-based vaccine or therapy. If vaccines could have lower doses, vaccine manufacturers could produce more doses within a shorter period of time. According to Settembre, there is also “the potential to drop the reactogenicity of whatever the intervention is.”
The effect of a therapy can also be extended over a longer period of time with sa-mRNA. In most existing mRNA-based therapies, protein expression is highest the first day and then drops over the following days. “For the sa-mRNA, the protein expression increases for about seven days after receiving an sa-mRNA-based vaccine,” Settembre continues. “So, there is a somewhat prolonged expression.”
The use of an sa-mRNA vaccine also triggers a stronger immune system attack. Like other mRNA vaccines, sa-mRNA vaccines can be used to create antibodies against a disease. In addition, sa-mRNA vaccines stimulate CD8-positive T cells, which are cytotoxic, to join the fight.
Getting mRNA deep in the lungs
Like any therapy, the method of delivery plays a crucial role in using mRNA-based methods. At Emory University School of Medicine, Philip Santangelo, PhD, an associate professor of bioengineering, studies ways to treat the lungs with mRNA-based therapies.

Associate Professor, Bioengineering
Emory University School of Medicine
“Back in 2016,” Santangelo recalls, “we proposed to DARPA using mRNA to deliver antibody-encoding mRNA to the lungs.” At that time, he was trying to deliver the mRNA by using an intratracheal water spray instillation of mRNA-encapsulating polyethyleneimine-based nanoparticles.
To turn this concept into a clinical application, Santangelo started thinking about using a nebulizer to deliver the mRNA. The treatment, he explains, needs to get deep in the lungs, because “people die from lower respiratory infections, not upper infections.”
In studies with rodents, Santangelo’s team uses an Aerogen Solo or Aerogen Pro to deliver the mRNA formulation. “We made our own nose-only setups for delivery as they have very small dead volumes and allow us to screen formulations in vivo in rodents using very little material,” he notes. “This is a huge advantage for screening formulations.”
Tests in other animals require different approaches. In ferrets, for example, the researchers use a long tube with a nebulizer on the end. “For nonhuman primates,” Santangelo continues, “we use a pediatric mask and nebulizer—very similar to what is used in humans.”
Santangelo says that the mRNA used in the tests is “typically either formulated in lipid nanoparticles via microfluidics or with polymers via simple mixing prior to nebulization.” He adds, “We have lyophilization protocols for our polymer.”
Santangelo envisions using such treatments for a range of diseases, from bacterial and viral infectious diseases to various lung diseases, including pulmonary arterial hypertension and pulmonary fibrosis. Most recently, Santangelo and his team started treating the lung with mRNA that encodes for Cas13, which is a programmable RNase for targeting flu and SARS-CoV-2.
“We deliver an mRNA that encodes for Cas13 in addition to a guide targeted to the virus in question,” he details. “We’ve seen that [using a nebulizer to deliver the polymer-formulated RNA] can be very effective for targeting RNA viruses in the lung.” Changing the guide allows the treatment to be switched from influenza to COVID-19. Also, both guides can be deployed. Indeed, Santangelo reports that his team is “making a version that targets both influenza and SARS-CoV-2 at the same time.” That allows very efficient processing.
Cancer solutions from synthetic biology
Scientists and companies apply a wide variety of technologies, including mRNA, in hopes of developing new cancer treatments. “There are multiple advantages of using mRNA to treat cancer, because mRNA expresses more efficiently and is also safer than viral gene therapy vectors,” says Tasuku Kitada, PhD, co-founder, president, and head of R&D at Strand Therapeutics. “When compared to DNA-based approaches, mRNA does not need to enter the nucleus.” That’s one less challenge when using mRNA-based cancer treatments.

Co-Founder, President, Head of R&D, Strand Therapeutics
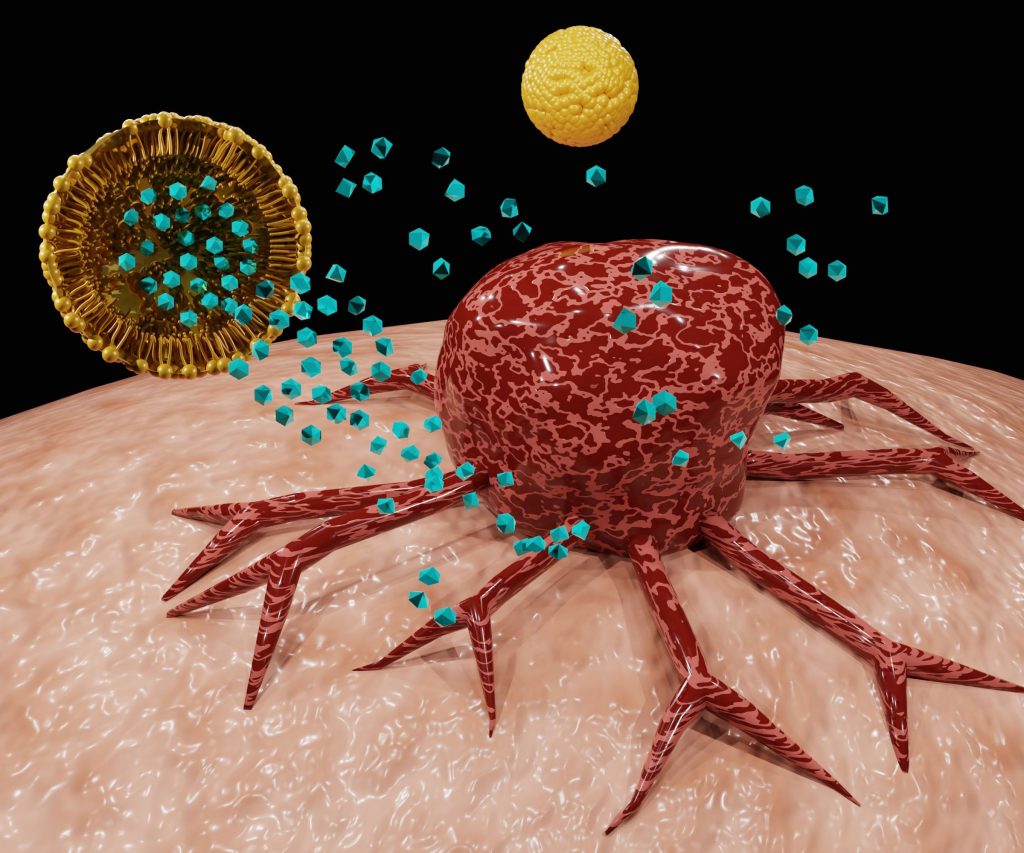
The question is: How can mRNA be used most effectively against cancer? “Many companies are using mRNA to develop cancer vaccines or expressing cytokines, antibodies, and other factors that have anticancer effects,” Kitada explains. “However, the problem with using these approaches is the risk of significant side effects.” So, scientists at Strand use synthetic biology methods to develop mRNA-based therapeutics that reduce this problem. Kitada points out that Strand’s technology allows “mRNA therapeutics to ‘sense’ biomarkers found in cancer cells and express proteins only inside cancer cells.”
To create these very specific and targeted treatments, Strand scientists create programmable, long-acting mRNA therapeutics that will be delivered in nanoparticles. The result, says Kitada, is the ability to “precisely control the location, timing, and expression level of mRNA within the patient.” Consequently, Strand’s cancer therapies should be less toxic to patients.
Current treatments under development include ones for solid tumors, such as melanoma and triple-negative breast cancer, as well as ones for blood-based cancers, including non-Hodgkin’s lymphoma.
Tomorrow’s treatments
Given the success of using mRNA against COVID-19 and the projects described here, many experts in healthcare expect even more powerful mRNA-based treatments ahead. Nonetheless, lots of work remains to be done, including much more basic research as well as an extensive number of clinical trials.
“It’s still early days for the field of mRNA-based treatments,” Settembre says. “There are so many improvements that we can make.”



