SARS-CoV-2 is known to infect cells of the respiratory tract. A deeper understanding of which cells support the infection, and to what extent, could lead to insights into disease progression and severity. Scientists at the UNC School of Medicine sought to understand which cells in the airway the virus infects, and how it gets into the lungs in the patients who develop pneumonia. To this end, they have characterized some of the ways in which SARS-CoV-2 infects the nasal cavity and infects and replicates progressively less well in cells lower down the respiratory tract—including the lungs.
The team’s findings suggest the virus tends to become firmly established first in the nasal cavity, but in some cases the virus is aspirated into the lungs, where it may cause more serious disease, including potentially fatal pneumonia.
The results are published in Cell in the paper, “SARS-CoV-2 Reverse Genetics Reveals a Variable Infection Gradient in the Respiratory Tract.”
“If the nose is the dominant initial site from which lung infections are seeded, then the widespread use of masks to protect the nasal passages, as well as any therapeutic strategies that reduce virus in the nose, such as nasal irrigation or antiviral nasal sprays, could be beneficial,” said study co-senior author Richard Boucher, MD, a professor of medicine and director of the Marsico Lung Institute at the UNC School of Medicine.
“This is a landmark study that reveals new and unexpected insights into the mechanisms that regulate disease progression and severity following SARS-CoV-2 infection,” said Ralph Baric, PhD, professor of epidemiology at the UNC Gillings School of Public Health. “In addition,” Baric continued, “we describe a new reverse genetic platform for SARS-CoV-2 allowing us to produce key indicator viruses that will support national vaccine efforts designed to control the spread and severity of this terrible disease.”
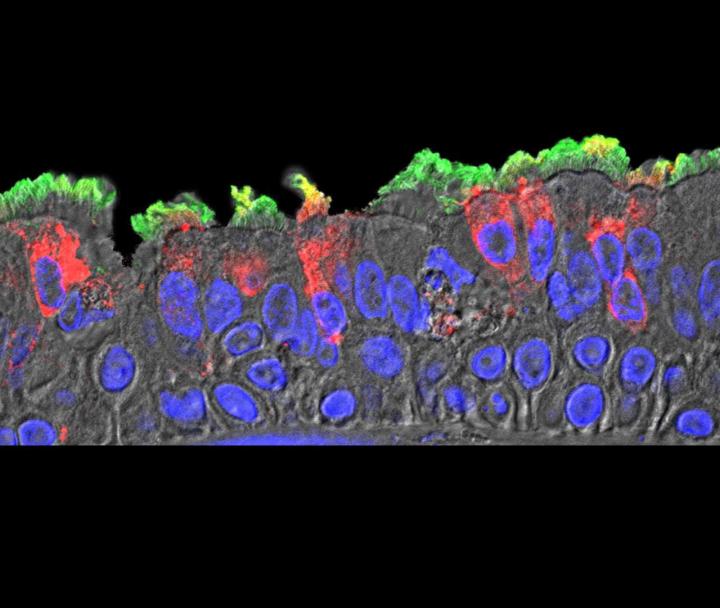
The researchers used a reverse genetics system to generate a GFP reporter virus to explore SARS-CoV-2 pathogenesis. The authors wrote that “high-sensitivity RNA in situ mapping revealed the highest ACE2 expression in the nose with decreasing expression throughout the lower respiratory tract, paralleled by a striking gradient of SARS-CoV-2 infection in proximal (high) vs distal (low) pulmonary epithelial cultures.”
The researchers used different isolates of SARS-CoV-2 to see how efficiently they could infect cultured cells from different parts of the human airway. They found a striking pattern of continuous variation, or gradient, from a relatively high infectivity of SARS-CoV-2 in cells lining the nasal passages, to less infectivity in cells lining the throat and bronchia, to relatively low infectivity in lung cells.
ACE2—the cell surface receptor that the virus uses to get into cells—was found to be more abundant on nasal-lining cells and less abundant on the surface of lower airway cells. This difference could explain, in part, why upper airway nasal-lining cells were more susceptible to infection.
Other experiments focused on TMPRSS2 and furin, two protein-cleaving enzymes found on many human cells. It’s thought that SARS-CoV-2 uses those two enzymes to re-shape key virus proteins and enter human cells. The experiments confirmed that when these human enzymes are more abundant, this particular coronavirus has an increased ability to infect cells and make copies of itself.
From studies done on autopsied lungs from COVID-19 patients, the team “identified focal disease and, congruent with culture data, SARS-CoV-2-infected ciliated and type 2 pneumocyte cells in airway and alveolar regions, respectively.” These findings, they wrote, “highlight the nasal susceptibility to SARS-CoV-2 with likely subsequent aspiration-mediated virus seeding to the lung in SARS-CoV-2 pathogenesis.”
Intriguingly, the virus did not infect airway-lining cells called club cells, despite the fact that these cells express both ACE2 and TMPRSS2. Moreover, the same types of airway epithelial cells from different human donors, especially lower-airway epithelial cells, tended to vary significantly in their susceptibility to infection. Such findings suggest that there are undiscovered factors in airway cells that help determine the course of infection in individuals—a course known to vary widely from mild or no symptoms all the way to respiratory failure and death.
The team mapped the sites of coronavirus infection in the lungs of several people who had died from COVID-19, and found that these sites exhibited a sort of patchiness and other characteristics consistent with the hypothesis that these sites had originated from infection higher in the airway.
The hypothesis that aspiration of oral contents into the lung is a significant contributor to COVID-19 pneumonia is consistent with the observations that people at higher risk for severe lung disease—the elderly, obese, and diabetic—are more prone to aspiration, especially at night.
The team also found that previously described individual antibodies capable of neutralizing the original SARS coronavirus of 2002 and the MERS coronavirus, which has been spreading slowly in the Middle East since 2012, did not neutralize SARS-CoV-2. However, blood serum from two of five SARS 2002 patients showed a low level but significant capability to neutralize SARS-CoV-2 infectivity in cultured cells. These data suggest that people who have been exposed to other coronaviruses may carry some other types of antibodies in their blood that provide at least partial protection against SARS-CoV-2.
“These results,” noted James Kiley, director of the division of lung diseases at the National Heart, Lung, and Blood Institute, “using some novel and innovative methodology, open new directions for future studies on SARS-C0V-2 that may guide therapeutic development and practices for reducing transmission and severity of COVID-19.”