Immunotherapy, which uses the body’s own immune system to fight cancer, can be an effective treatment option, yet many patients do not respond to it. Cancer researchers are seeking new ways to optimize immunotherapy so that it might be more effective for more people.
It has previously been thought that cancer cells do not rely heavily on mitochondria, despite still having oxygen and sugars available to them to fuel mitochondrial metabolism. This hypothesis dominated the field of cancer metabolism until recently, when scientists found that mitochondria actually do play multiple important roles in tumor growth.
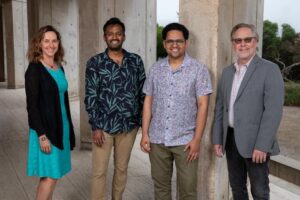
Kaech and co-senior study author Gerald Shadel, PhD, teamed up to better understand how mitochondria influence both tumor growth and the way in which the immune system recognizes and responds to cancer. Shadel holds the Audrey Geisel Chair in Biomedical Science, and director of the San Diego Nathan Shock Center of Excellence in the Basic Biology of Aging.
“We wanted to better understand how tumors acquire the metabolic state that gives them a growth advantage as well as an ability to evade the immune system, which I call the ‘double whammy,’” said Susan Kaech, PhD, director of the NOMIS Center for Immunology and Microbial Pathogenesis. “And we found a way to make the tumors more recognizable by the immune system and potentially more responsive to immunotherapy.” Kaech is co-senior author of the researchers’ published paper in Science, titled “Manipulating mitochondrial electron flow enhances tumor immunogenicity.” In their paper the team concluded, “… this ETC-rewiring approach might represent a one-two punch to convert cold tumors to hot and to improve antitumor responses and immunotherapy efficacy.”
For their study, the investigators altered a key step in the electron transport chain, the process that moves electrons through mitochondria, and which ultimately leads to production of adenosine phosphate (ATP), the main energy-providing molecule in cells.
There are two primary routes by which electrons flow inside mitochondria to initiate ATP production. The “gatekeepers” for these two routes are known as complex I (CI) and complex II (CII). As the team explained in their paper, “Although tumor growth requires the mitochondrial electron transport chain (ETC), the relative contribution of complex I (CI) and complex II (CII), the gatekeepers for initiating electron flow, remains unclear.”
To investigate the contributions of CI and CII to tumor growth and antitumor responses the team knocked out either CI or CII in mouse melanoma cells, that were then implanted into experimental mice.
They observed that tumors in which CII, but not CI, was knocked out were more slow growing. “Unexpectedly, CI and CII knockout had notably differential effects on tumor growth …” the team noted. “.… CII knockout tumors grew significantly slower compared with control and CI knockout tumors.” Significantly, CII knockout tumors also showed increased immune cell infiltration, especially CD8+ immune cells, relative to control and CI knockout tumors.
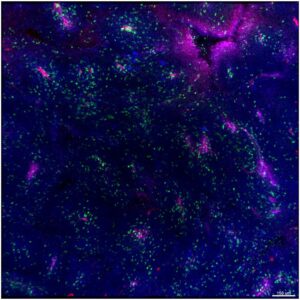
Further investigation showed that knocking out CII and so forcing electrons to primarily go through just one of the ETC routes led to overproduction of the metabolite succinate. This accumulation of succinate led to expression of immune genes in the nucleus and increased the levels of a protein called MHC on the surface of the tumor cells. “We found significantly higher MHC-I expression on CII knockout tumor cells compared with CI knockout and control tumor cells in vivo,” they wrote. In turn, elevated levels of MHC made the tumor cells more visible to the specialized killer T immune cells that recognize and eliminate cancer cells.
While the team knew that the metabolic state of tumor cells dictated their enhanced growth properties, this new finding shows that relatively simple manipulations to mitochondrial electron transport can convert a tumor that is evading immune detection into one that is now highly susceptible to immune system attack. “There’s an explosion of recent research activity from my lab and others revealing how mitochondria regulate the immune system and inflammation, and this study highlights an exciting new chapter in this story,” said Shadel.
The authors added, “… we conclude that the loss of CII, but not of CI, results in a strong antitumor T cell response through increased antigen presentation.” The collective results indicate that increasing intracellular tumor succinate and MHC-1 by inhibiting CII enhances tumor cell immunogenicity and the activation and infiltration of tumor-reactive CD8+ T cells that suppress tumor growth. “Our results indicate that discrete rewiring of the ETC to moderately reduce CII activity or increase succinate in tumors not only improves T cell engagement by increasing MHC-I but also enhances the selective expansion of protective T cell clones, which suggests that tumor MHC-I levels determine tolerogenic versus immunogenic set points for tumor antigens.”
“We were surprised to find that mitochondrial activity determines how susceptible a tumor is to being recognized by the immune system,” commented co-first author Kailash Chandra Mangalhara, PhD, a senior research associate in Shadel’s lab. We think we found a novel mechanism by which antigen presentation in tumor cells is regulated. These findings change how we now think about future treatment strategies.”
The researchers plan to explore ways to leverage the newly identified mechanism to fight cancer without harming mitochondria, which can have adverse effects on normal cells. They will continue to study the role of mitochondrial metabolism in cancer, immune responses, and immunotherapy efficacy.


