Researchers headed by teams at the Salk Institute and at the University of California, San Diego (UCSD), have discovered, in mice, how high-fat diets (HFDs) can change gut bacteria and alter digestive molecules called bile acids that are modified by those bacteria, predisposing the animals to colorectal cancer.
The study found increased levels of specific gut bacteria in mice fed HFDs, and indicated that those gut bacteria alter the composition of the bile acid pool in ways that cause inflammation and affect how quickly intestinal stem cells replenish. Reporting on their study in Cell Reports, the investigators suggest that their findings could have utility in future diagnostic and therapeutic approaches to gastrointestinal cancer.
“The balance of microbes in the gut is shaped by diet, and we are discovering how alterations in the gut microbial population (the gut microbiome) can create problems that lead to cancer,” said Ronald Evans, PhD, director of Salk’s Gene Expression Laboratory. “This paves the way toward interventions that decrease cancer risk.” Evans is co-senior author of the team’s published paper, titled “Paired microbiome and metabolome analyses associate bile acid changes with colorectal cancer progression.” In their report, the team stated, “In general, the modulation of gut microbiota and BA profiles holds promise as a novel therapeutic approach for the treatment of gastrointestinal cancers and represents the next frontier for gastrointestinal cancer research.”
The prevalence of colorectal cancer (CRC) in people under 50 years of age has risen in recent decades, and one suspected reason is the increasing rate of obesity and high-fat diets. The authors noted that colorectal cancer now represents the fourth leading cause of cancer-related deaths worldwide, and with an expected increase in incidence over the coming decades, new diagnostic and treatment approaches are needed.
“Diet and lifestyle choices” have been identified as risk factors for CRC, and the authors further cite figures suggesting that about 50–60% of cases in the United States are attributed to modifiable risk factors. “However, the convergence of environmental and genetic factors in the development and progression of CRC is not fully understood,” they pointed out.
Bile acids are molecules produced by the liver and used by the gut to help digest food and absorb cholesterol, fats, and nutrients. In 2019, Evans and his colleagues showed in mice how high-fat diets boosted overall bile acid levels. The shift in bile acids, they found, shut down a key protein in the gut—called the Farnesoid X receptor (FXR)—and increased the prevalence of cancer. However, there were still missing links in the story, including how the gut microbiome and bile acids are changed by high-fat diets.
For the newly reported work Evans’ group teamed up with the labs of Rob Knight, PhD, and Pieter Dorrestein, PhD, at UCSD to examine the microbiomes and metabolomes—collections of dietary and microbially derived small molecules—in the digestive tracks of animals fed high-fat diets.

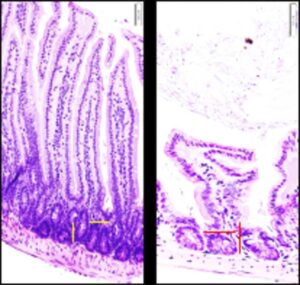
The scientists applied techniques including metagenomic and paired metabolomic profiling to study diet-related changes in the gut microbiomes, and the consequences of those changes, in engineered mice (APCmin/+ animals) with a genetic mutation that makes them more susceptible to colorectal tumors. There were four test groups of animals. APCmin/+ animals fed either a normal diet (ND), or HFD, and wild-type (WT) mice fed either a normal diet, or HFD.
The analyses showed that while mice fed high-fat diets had more bile acids in their guts, it was a less diverse collection with a higher prevalence of certain bile acids that had been changed by gut bacteria.
There were also striking differences in the microbiomes of the mice on high-fat diets. The collections of gut bacteria in these animals’ digestive tracts were less diverse and contained different bacteria when compared with the microbiomes of mice not on HFDs. “Of note, species of the genus Prevotellaceae were more associated with the APCmin/+ genotype, while species of the family Lachnospiraceae were more associated with the WT genotype,” the scientists stated. “On the diet side, species of the family Erysipelotrichaceae were more associated with HFD, while species of the family ClostridiaceaeI were more associated with ND.” In addition, they pointed out, “non-classic amino acid conjugation of the bile acid cholic acid (AA-CA) increased with HFD.” Two of the identified bacteria—Ileibacterium valens and Ruminococcus gnavus—were able to produce these modified AA-CA bile acids.
The scientists were surprised to discover that a high-fat diet actually had a greater impact on the microbiome and modified bile acids than a genetic mutation that increases cancer susceptibility in the animals. “Using this APCmin/+ mouse model of CRC, we show here that the effects of an HFD on the cecum microbiome are more pronounced than those from the genetic mutation, significantly reducing microbial α diversity and perturbing the metabolome,” they wrote.
They also discovered that these modified bile acids affected the proliferation of stem cells in the intestines. When these cells don’t replenish frequently they can accumulate mutations, which is a key step toward encouraging the growth of cancers that can often arise from these stem cells. We show that AA-CAs impact intestinal stem cell growth and demonstrate that Ileibacterium valens and Ruminococcus gnavus are able to synthesize these AA-Cas,” they further pointed out.
“We’ve pinpointed how high-fat diet influences the gut microbiome and reshapes the bile acids pool, pushing the gut into an inflamed, disease-associated state,” added co-first author Ting Fu, PhD, a former postdoctoral fellow in the Evans lab.
The researchers believe high-fat diets change the composition of the microbiome, encouraging the growth of bacteria like I. valens and R. gnavus. In turn, that boosts levels of modified bile acids. In a vicious cycle, those bile acids create a more inflammatory environment that can further change the makeup of gut bacteria.
“We’ve deconstructed why high-fat diets aren’t good for you, and identified specific strains of microbes that flare with high-fat diets,” said Evans, the March of Dimes chair in molecular and developmental biology. “By knowing what the problem is, we have a much better idea of how to prevent and reverse it.” Added co-author Michael Downes, PhD, at Salk, “We are only just beginning to understand these bacterially-conjugated bile acids and their roles in health and disease.”
Commenting on their results, the team stated, “This study demonstrates the combinatorial effects of genetic and dietary risk factors on the gut microbiome and metabolome. Our results show that both genetic and dietary risk factors contribute to the alterations in the serum and cecum metabolome profiles … Our multi-omics analyses also show that diet is the strongest driver of microbemetabolite interactions, especially so in the identified BA.”
The scientists aim to study how quickly the microbiome and bile acids change after an animal begins eating a high-fat diet. They also plan to study ways to reverse the cancer-associated effects of a high-fat diet by targeting FXR—the protein that they previously discovered to be associated with bile acid changes.