Among all ovarian cancers, the worst prognosis is seen in ovarian clear cell carcinomas (OCCC) which typically don’t respond to chemotherapy. Over half of the patients with OCCC harbor loss-of-function mutations in the tumor suppressor gene, ARID1A. The gene ARID1A provides instructions for making a protein that forms an integral component of several different SWI/SNF protein complexes that regulate gene expression by remodeling chromatin.
A new study shows ARID1A mutations abnormally increase a cell’s dependence on glutamine metabolism. This is because ARID1A is part of an SWI/SNF protein complex that represses the broadly expressed gene glutaminase (GLS1)—an enzyme that hydrolyzes the amino acid glutamine to glutamate. ARID1A inactivating mutations remove this homeostatic repression.
The study also shows that pharmacologically inhibiting glutamine metabolism with or without immune checkpoint blockade may constitute an effective therapeutic strategy for ARID1A-mutant ovarian cancer.
These findings are reported in the article titled, “Targeting glutamine dependence through GLS1 inhibition suppresses ARID1A-inactivated clear cell ovarian carcinoma,” published in Nature Cancer.
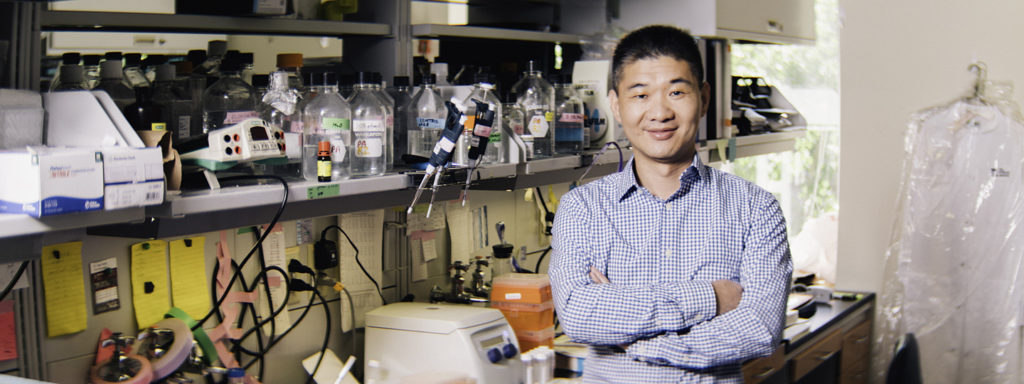
“Metabolic reprogramming is a hallmark of many cancers, including OCCC. In this study we assessed whether ARID1A plays a role in regulation of metabolism,” said Rugang Zhang, PhD, deputy director of the Wistar Institute Cancer Center, professor and leader of the immunology, microenvironment & metastasis program, and corresponding author on the paper. “We found that its inactivation in cancer cells creates a specific metabolic requirement for glutamine and exposed this as a vulnerability that could be exploited for therapeutic purposes.”
Treating ARID1A mutant and control cells with the glutaminase inhibitor CB-839 suppresses the growth of ARID1A mutant but not control cells, the authors reported. Glutamine is normally required for cancer cells to grow, but Zhang and colleagues demonstrated a stronger dependence of ARID1A-mutant cells on this amino acid.
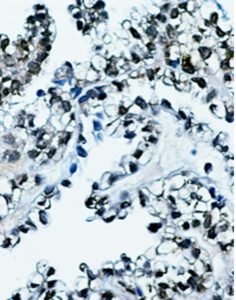
The authors investigated the transcriptional effect of ARID1A inactivation and found that GLS1 was the top upregulated gene among those controlling glutamine metabolism. GLS1 was expressed at significantly higher levels in tumor samples from patients with other cancer types as well, which also carry mutations in the SWI/SNF complex.
Increased glutamine dependence correlates with an increase in the utilization of glutamine in the respiratory tricarboxylic acid cycle to generate aspartate, essential for nucleotide synthesis. “ARID1A may also regulate other metabolic pathways that utilize intermediate glutamine metabolites, which together with GLS1 upregulation confers sensitivity to GLS inhibitor,” the authors noted.
The team evaluated the therapeutic potential of inhibiting the glutamine metabolism by blocking the glutaminase enzyme with the well-established CB-839 inhibitor. This molecule is under investigation in clinical trials and is well tolerated as a single agent and in combination with other anticancer therapies.
CB-839 significantly reduced tumor burden and prolonged survival of OCCC mouse models. These studies were expanded to mice carrying patient-derived tumor transplants, confirming that CB-839 impaired the growth of ARID1A-mutant but not ARID1A-wildtype tumors.
Glutamine metabolism regulates immune lymphocyte function in the tumor microenvironment. Earlier studies that show ARID1A mutation confers sensitivity to immune checkpoint blockades, such as anti-PD-L1, and glutamine antagonism in effector T cells can be exploited as a “metabolic checkpoint.” These earlier studies propelled the authors to investigate whether CB-839 synergizes with anti-PD-L1 in the immune-competent OCCC genetic mouse model.
Anti-PD-L1 treatment alone only has a modest effect on improving survival of mice bearing ARID1A-inactivated tumors. However, combined CB-839 with anti-PDL1 treatment in the current study revealed a synergy between glutaminase inhibitors and immune checkpoint blockade in suppressing the growth of ARID1A-mutant OCCC tumors.
Not only does a deficiency of functional ARID1A increase dependence on glutamine dependence, it also decreases glucose uptake, the study reported. “These findings suggest that inactivation of the SWI/SNF complex reprograms metabolic pathway from glycolysis to glutamine dependence,” the authors noted.
“Our findings suggest that glutaminase inhibitors warrant further studies as a standalone or combinatorial therapeutic intervention for OCCC, for which effective options are very limited,” said Shuai Wu, PhD, first author of the study and a staff scientist in the Zhang Lab.
Glutaminase inhibitors could become a new strategy to precisely target a specific vulnerability of OCCC cells associated with loss of ARID1A function. This is a personalized therapeutic strategy because ARID1A mutation serves as a biomarker, whereas ARID1A–repressed GLS1 serves as ARID1A mutation-dependent therapeutic target.