A method has been reported by researchers from Tsinghua University in China, which enables the efficient and high-throughput production of lung cancer assembloids. These assembloids are three-dimensional structures that encapsulate tumor microenvironment cells derived from patients’ tumors and lung cancer organoids within microgels. The lung cancer assembloids not only reproduce the molecular, cellular, and functional diversity of the original tumors, but also accurately mimic the clinical outcomes of patients. This indicates that the cancer assembloid model has the potential to predict personalized treatments. The utilization of this model and subsequent modifications has the potential to stimulate clinical-translational endeavors aimed at the advancement of combination therapies and personalized therapy for lung cancer.
The research article, “A patient-specific lung cancer assembloid model with heterogeneous tumor microenvironments,” was published in Nature Communications.
Tumor microenvironments influence clinical outcomes
Cancer models are of utmost importance in fundamental cancer research, the advancement of anticancer drugs, and precision medicine. Nevertheless, conventional cancer models, such as two- and three-dimensional cultures, are deficient in capturing the diverse cell subtypes and molecular characteristics found in parental tumors. Additionally, they are constrained by their incapacity to replicate the intricate three-dimensional structure and varied tumor microenvironments observed in in vivo tumors.
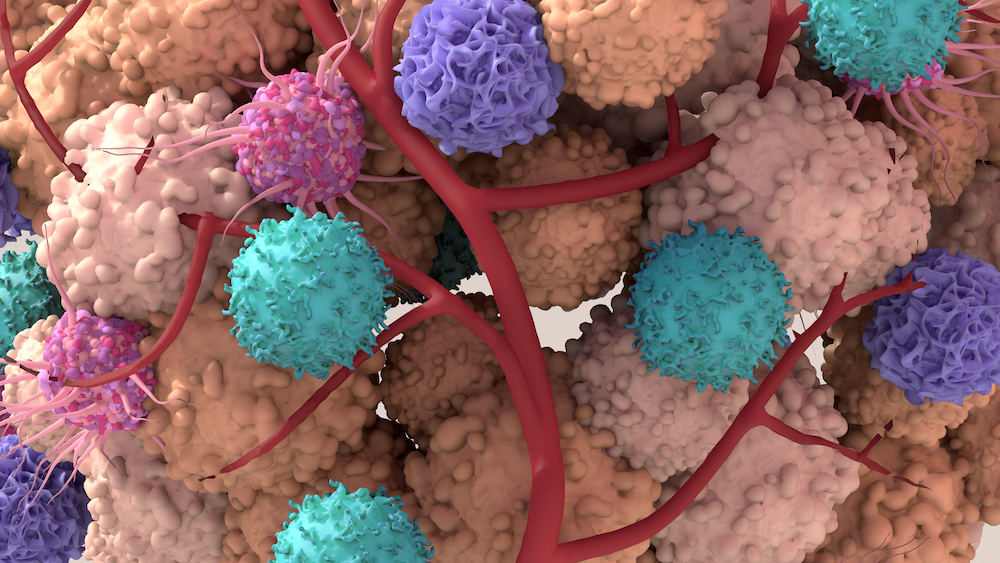
The microenvironment of tumors plays a crucial role in determining the therapeutic response and clinical outcome. The utilization of 3D cancer models incorporating the tumor microenvironment is of utmost importance in comprehending the progression of cancer and in the advancement of therapeutic agents targeting cancer. While several 3D methodologies have been devised to simulate the tumor microenvironment, including self-assembling spheroids, organoid coculture, and organotypic models, their widespread utilization is hindered by the absence of patient-specific tumor microenvironment, time-consuming processes, and inadequate intra-batch consistency.
The patient-specific lung cancer assembloid model
Assembloids are three-dimensional structures that arise from the amalgamation and functional integration of various cell types or organoids. These structures have emerged as cutting-edge tools in stem cell research, offering valuable insights into human development and disease. For example, bladder tumor assembloids accurately replicated the in vivo pathophysiological characteristics of urothelial carcinoma to some extent. The study conducted by Yanmei Zhang, Qifan Hu, and Yuquan Pei focused on creating a novel lung cancer assembloid model tailored to individual patients. This model was developed using droplet microfluidic technology based on a microinjection strategy.
The approach devised by researchers from Tsinghua University involves the uniform encapsulation of tumor microenvironment cells derived from patients’ tumors and lung cancer organoids within gelatin microgels. The researchers demonstrated that this approach facilitated accurate manipulation of clinical microsamples and efficient production of lung cancer assembloids, exhibiting consistent size and cell composition within each batch. This was accomplished by evenly enclosing tumor microenvironment cells obtained from patients’ tumors and lung cancer organoids within microgels. Furthermore, the lung cancer assembloids serve as a representation of the tumor microenvironment and tumor heterogeneity found in their parental tumors. Additionally, they accurately mimic the clinical responses observed in patients with lung cancer. This underscores the potential usefulness of our lung cancer assembloid model for fundamental research and personalized drug screening.
The researchers from Tsinghua University conducted a systematic comparison between the accuracy of drug testing results based on lung cancer assembloids and the actual clinical outcomes of patients. They also evaluated the potential of lung cancer assembloids as a preclinical model for personalized drug testing. In contrast to lung cancer organoids, lung cancer assembloids can replicate the tumor microenvironments of patients, encompassing diverse cancer-associated fibroblasts and the tumor immune microenvironment. This replication facilitates the development of tumor-like morphology.
Lung cancer assembloids and lung cancer organoids exhibited distinct reactions to chemotherapeutic and targeted drugs due to the existence of tumor microenvironments. In the future, it is imperative to undertake further comparisons between lung cancer organoids and lung cancer assembloids, employing larger sample sizes. Furthermore, the utilization of the lung cancer assembloid model has demonstrated its ability to effectively forecast the clinical treatment outcomes of patients undergoing neoadjuvant immunotherapy in conjunction with chemotherapy and targeted therapy.
These studies offer a valuable approach for accurately creating cancer assembloids and a promising model for cancer research and personalized medicine. It is noteworthy that the lung cancer assembloids generated using this hydrogel exhibit the ability to undergo cryopreservation and thawing processes with minimal harm to the cells and shapes of the lung cancer assembloids. This observation implies that lung cancer assembloid models have the potential to be preserved and utilized for future research endeavors.