Glioblastoma, also known as glioblastoma multiforme (GBM), is the most aggressive type of cancer that begins within the brain. Only 25% of patients with this type of brain tumor survive for more than one year and just 5% live for more than five years.
Now, a team at the Brain Tumor Research Centre of Excellence at Queen Mary University of London has uncovered new insights into how GBM develops, identifying potential new targets for individualized treatments.
Their findings are published in the journal Nature Communications, in a paper titled “Comparative epigenetic analysis of tumor initiating cells and syngeneic EPSC-derived neural stem cells (SYNGN) in glioblastoma.”
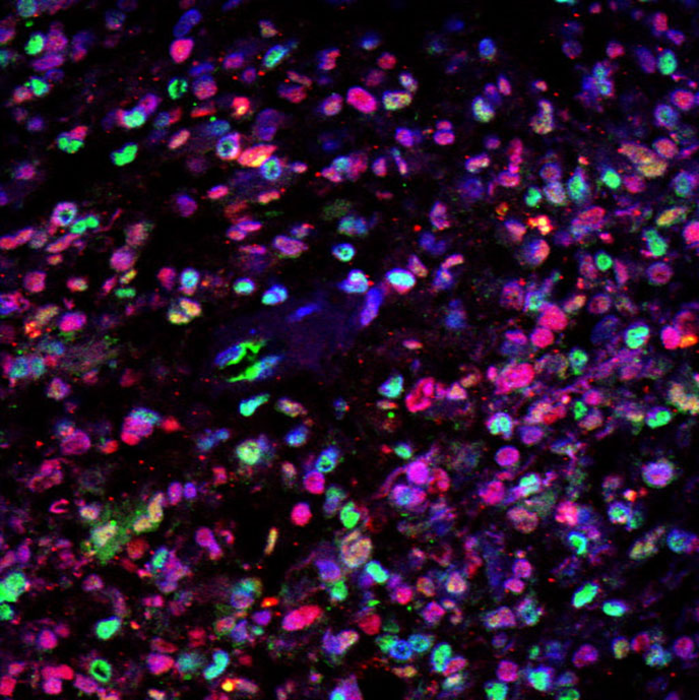
“Epigenetic mechanisms which play an essential role in normal developmental processes, such as self-renewal and fate specification of neural stem cells (NSC) are also responsible for some of the changes in the GBM genome,” the researchers wrote. “Here we develop a strategy to compare the epigenetic and transcriptional make-up of primary GBM cells (GIC) with patient-matched expanded potential stem cell (EPSC)-derived NSC (iNSC).”
The researchers developed an approach to generate syngeneic neural stem cells and use them as patient-specific comparators to glioma initiating cells for the discovery of pathogenetically relevant mechanisms in glioblastoma and to identify druggable targets in patients.
“We have used this powerful technique to identify changes in the function of genes that occur in GBM that do not entail a change in the genetic code (epigenetics), explained Silvia Marino, MD, professor neuropathology.”This has revealed new insights for how GBM develops and identified potential new targets for individualized treatments.”
The researchers identified significant molecular differences which could be used to develop new treatments.
Hugh Adams, spokesman for Brain Tumor Research, said: “The complex nature of this particular tumor type means that the standard of care for these patients has not changed in a generation so this research brings much-needed hope for the future. One of the main challenges in developing effective treatments for GBM is that the tumor exhibits significant variation between patients and there can even be significant variation within a single patient’s tumor. These variations can arise from changes to the cell’s genetic code—known as mutations—combined with changes to how specific genes are controlled.
“There is strong evidence that GBM cells develop from neural stem cells but previous studies have not been able to compare tumor cells and their putative cell of origin from the same person. Marino and her team have now harnessed state-of-the-art stem cell technologies and next-generation DNA sequencing methods to compare diseased and healthy cells from the same patient. Their results have shown how this approach can reveal novel molecular events that appear to go awry when GBM develops, thereby identifying targets for potential new treatments.”
“Our approach has identified functionally relevant epigenetic modifications of target genes that predict differential response to drugs currently in clinical use, which could be trialed for GBM treatment,” concluded the researchers.