Immunotherapeutics have shown great promise. However, their response rate for many types of cancers is low. Researchers at Massachusetts General Hospital (MGH) sought to determine the impact of carcinogen exposure on cancer development. They found how cells exposed to certain carcinogens become immunogenic, and how that exposure might be exploited to treat cancers such as breast and other epithelial cancers.
Their findings are published in the journal Science Advances in a paper titled, “CD8+ T cell immunity blocks the metastasis of carcinogen-exposed breast cancer.”
“The link between carcinogen exposure and cancer immunogenicity is unclear,” wrote the researchers. “…To determine the impact of carcinogen exposure on breast cancer development, we treated PyMT mice with a single oral dose of 1 mg of DMBA or olive oil (carrier) at puberty and before the onset of breast tumorigenesis. After DMBA or olive oil treatment, mice were monitored weekly for any sign of breast cancer development.”
The researchers discovered that the mechanism involves stimulating the release of small proteins known as chemokines which recruit CD8+ T cells to the tumor site to block metastasis, potentially enhancing the effectiveness of a new generation of immunotherapies.
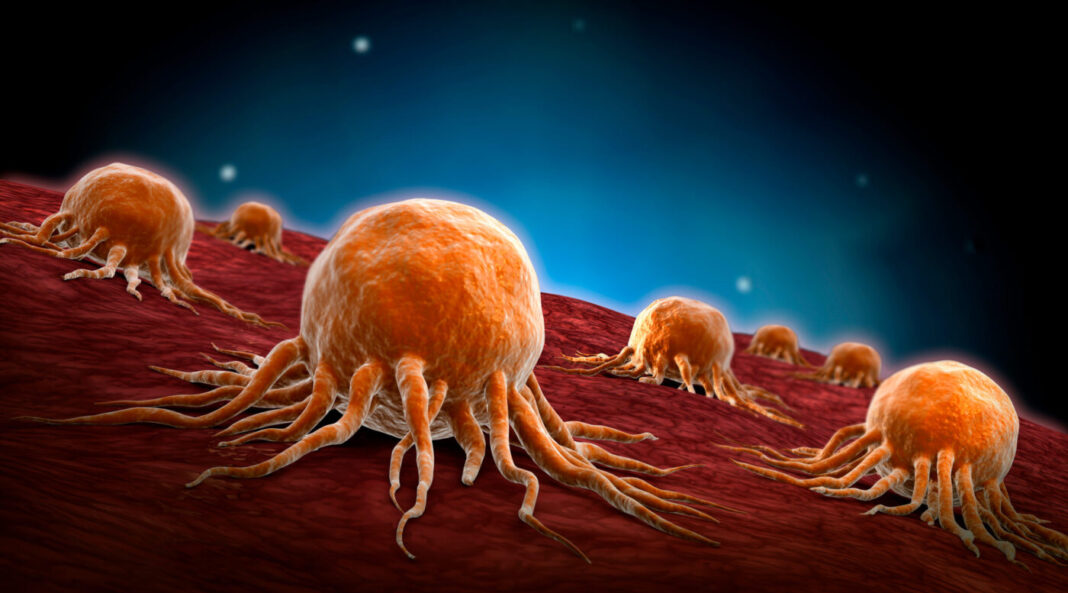
CD8+ T cells are major drivers of antitumor immunity and effectively attack cells exposed to environmental carcinogens.
In mouse study, the MGH team demonstrated for the first time another consequence of carcinogen exposure that can have significant immunologic implications, namely, the nongenetic alteration of cells through such harmful environmental factors as smoking, ultraviolet light, and pollution.
“This finding is particularly important because it could open the door to therapeutic interventions that aren’t practical with a DNA approach, since no clinician wants to introduce even more genetic mutations into cancer cells just to make them more immunogenic,” explained Demehri. “We learned if there was another immunogenic element associated with carcinogen exposure independent of or even complementary to the presence of the mutation, then you could deliver that factor into a ‘cold’ tumor to make it ‘hot,’ meaning it would become immunogenic and responsive to immunotherapies.”
The factor is a chemokine known as CCL21. “Through its signaling, CCL21 recruits CD8+ T cells which infiltrate the tumor, as previous work has shown, and are associated with a significant reduction in relative risk of distant metastasis,” added lead author Kaiwen Li, MD, an investigator in MGH’s Center for Cancer Immunology, MGH’s Cutaneous Biology Research Center, and the department of urology at Sun Yat-sen Memorial Hospital at China’s Sun Yat-sen University. “Not only does CCL21 induce an antitumor immune response to prevent metastasis, but it overcomes other immune cells known as Tregs (immunosuppressive regulatory T cells) present in tumors from inhibiting the work of the CD8+ T cells.”
The researchers reported that an injection of CCL21 into the tumor might be able to transform cold breast cancers into hot tumors responsive to current immunotherapies.
“We hope that researchers will use these findings to open a much wider field of investigation into cancer immunology,” emphasized Demehri. “Specifically, studies are needed to identify the full array of cytokines and chemokines that are induced by environmental carcinogens in various types of cancers with the goal of harnessing the most potent mediators of antitumor immunity.”