Studies in mice have shown how cells called microglia may help to prevent the secondary progressive phase of multiple sclerosis (MS) by clearing dead cell debris, including myelin, from the central nervous system (CNS). Headed by scientists at the Karolinska Institutet, the research, in a mouse model of MS, found that this process of debris clearance—known as autophagy—was interrupted when a gene called Atg7 was removed from the microglia.
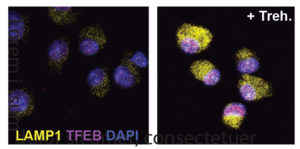
The experiments also showed that treating mice using the plant-derived sugar, trehalose, induced autophagy in microglial cells, and was associated with disease remission. “The treatment with trehalose shows that microglial cells can be targeted for beneficial purposes with a compound already found in plant- and fungi-derived diets—and thereby likely not toxic,” said Rasmus Berglund, doctoral student and lead author of the team’s published study. “This gives an option not only to use these findings as treatment of established disease but also the possibility of pro-active diet recommendations.”
Berglund and colleagues reported on their findings in Science Immunology, in a paper titled, “Microglial autophagy-associated phagocytosis is essential for recovery from neuroinflammation.”
MS is a chronic inflammatory disease of the CNS and one of the main causes of neurological functional impairment. The disease is generally diagnosed between 20 and 30 years of age, and can lead to severe neurological symptoms, such as loss of sensation and trembling, difficulties walking and maintaining balance, memory failure, and visual impairment. In the majority of cases, MS manifests as bouts with a certain amount of subsequent recovery. A gradual loss of function with time is, however, inevitable. Yet while disease progression is “the most clinically challenging” aspect of MS, it is also “the least mechanistically explored,” the investigators wrote.

“There is currently only one, recently approved, treatment for what is called the secondary progressive phase. The mechanisms behind this progressive phase require more research.”
Age is the strongest risk factor for developing progressive MS and many age-associated neurodegenerative diseases. Many other age-associated neurodegenerative pathologies, including Alzheimer’s disease, and autoinflammatory diseases such as Crohn’s disease, and systemic lupus erythematosus (SLE), are characterized by impaired autophagy, the process by which cells normally break down and recycle their own proteins and other structural components, including myelin in nerve cells.
In previous work, Berglund and colleagues had established a link between debris clearance in the CNS and disease severity in mice with experimental autoimmune encephalomyelitis (EAE), a common model of MS. The newly reported research in EAE mice found that recovery from brain inflammation depended on microglia performing debris-clearing functions in the CNS. The team’s studies showed that deleting a non-canonical autophagy gene Atg7 in the microglia of EAE mice led to accumulation of dead cell debris and propelled progressive MS-like disease. “Microglia-specific deletion of the autophagy regulator Atg7, but not the canonical macroautophagy protein Ulk1, led to increased intracellular accumulation of phagocytosed myelin and progressive MS-like disease,” the investigators wrote.
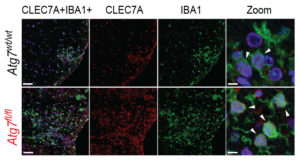
Conversely, triggering microglial cleaning functions in mice by giving the animals the disaccharide trehalose helped lead to disease remission, suggesting that the sugar should be further investigated for its therapeutic potential. “We herein demonstrate that a noncanonical form of autophagy in microglia is responsible for myelin degradation and clearance and that impairment of this pathway, which occurs during aging, contributes to the progression of MS-like disease,” the team concluded. “We show that we can modulate this process therapeutically, with implications in other age-related neuroinflammatory diseases.”
“The plant and fungi-derived sugar trehalose restores the functional breakdown of myelin residues, stops the progression, and leads to recovery from MS-like disease,” said Berglund. “By enhancing this process we hope one day to be able to treat and prevent age-related aspects of neuroinflammatory conditions.”



