![Two neonatal cardiomyocytes (stained red) undergoing cell division after treatment with NRG1 are shown. [Weizmann Institute of Science]](https://genengnews.com/wp-content/uploads/2018/08/Apr14_2015_WeizmannInstituteofScience_MouseNeonatalCardiomyocytes_HeartCell4590104955-1.jpg)
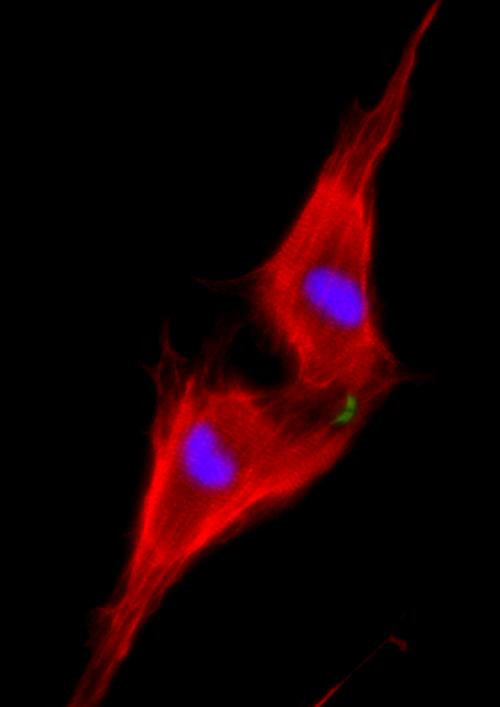
Two neonatal cardiomyocytes (stained red) undergoing cell division after treatment with NRG1 are shown. [Weizmann Institute of Science]
Adult heart cells have too little regenerative ability to replenish heart tissue that has suffered disease or injury—but just enough to encourage researchers, who keep trying to reinstate heart cells’ proliferative power, which mostly ebbs away after the first week of life. Many researchers are convinced that the best way to return adult heart cells to an earlier, regenerative state is to somehow stimulate the molecular pathways that heart cells use to accomplish cell division.
Following this approach, scientists at the Weizmann Institute of Science have found a way to restore the regenerative abilities of heart cells in adult mice. They took a close look at ERBB2, a receptor that works with a second, related, receptor by binding a growth factor called Neuregulin 1 (NRG1). Together, ERBB2 and NRG1 convey a growth signal and induce regeneration.
NRG1 has already been tested in clinical studies for treating heart failure. ERBB2, until now, has been better known for its ability to pass along growth signals that promote certain kinds of cancer. According to the Weizmann Institute scientists, however, it is a key link in the chain of molecular events that result in cardiac regeneration.
This finding appeared April 6 in Nature Cell Biology, in an article entitled, “ERBB2 triggers mammalian heart regeneration by promoting cardiomyocyte dedifferentiation and proliferation.”
Weizmann Institute researchers led by Prof. Eldad Tzahor wanted to know exactly how NRG1 and ERBB2 are involved in heart regeneration. In mice, new heart muscle cells can be added up to a week after birth; newborn mice can regenerate damaged hearts, while seven-day-old mice already cannot. The researchers observed that heart muscle cells called cardiomyocytes that were treated with NRG1 continued to proliferate on the day of birth; but the effect dropped dramatically within a week, even with ample amounts of NRG1. Further investigation showed that the difference between a day and a week was in the amount of ERBB2 on the cardiomyocyte membranes.
The team then created mice in which the gene for ERBB2 was knocked out only in cardiomyocytes. This had a severe impact: The mice had hearts with walls that were thin and balloon-like—a cardiac pathology known as dilated cardiomyopathy. The conclusion was that cardiomyocytes lacking ERBB2 do not divide, even in the presence of NRG1. Next, the team reactivated the ERBB2 protein in adult mouse heart cells, in which cardiomyocytes normally no longer divide. This resulted in extreme cardiomyocyte proliferation and hypertrophy—excessive growth of the individual cardiomyocytes—leading to a giant heart (cardiomegaly) that left little room for blood to enter. Too little or too much of this protein had a devastating impact on heart function.
The question then became: If one could activate ERBB2 for just a short period in an adult heart following a heart attack, might it be possible to get the positive results, that is, cardiac cell renewal, without such negative ones as hypertrophy and scarring? Testing this idea, the team found that they could, indeed, activate ERBB2 in mice for a short interval only following an induced heart attack and obtain nearly complete heart regeneration within several weeks. “The results were amazing,” said Prof. Tzahor. “As opposed to extensive scarring in the control hearts, the ERBB2-expressing hearts had completely returned to their previous state.”
Investigation of the regenerative process through live imaging and molecular studies revealed how this happens: The cardiomyocytes “dedifferentiate”—that is, they revert to an earlier form, something between an embryonic and an adult cell, which can then divide and differentiate into new heart cells. In other words, the ERBB2 took the cells back a step to an earlier, embryonic form; and then stopping its activity promoted the regeneration process.
“CM-specific Erbb2 knockout revealed that ERBB2 is required for CM proliferation at embryonic/neonatal stages. Induction of a constitutively active ERBB2 (caERBB2) in neonatal, juvenile and adult CMs resulted in cardiomegaly, characterized by extensive CM hypertrophy, dedifferentiation and proliferation, differentially mediated by ERK, AKT and GSK3β/β-catenin signaling pathways,” wrote the authors of the Nature Cell Biology article. “Transient induction of caERBB2 following myocardial infarction triggered CM dedifferentiation and proliferation followed by redifferentiation and regeneration.”
In continuing research, Prof. Tzahor and his team began to outline the pathway—the other proteins that respond to the NRG1 message inside the cell. “ERBB2 is clearly at the top of the chain. We have shown that it can induce cardiac regeneration on its own. But understanding the roles of the other proteins in the chain may present us with new drug targets for treating heart disease,” explained Gabriele D'Uva, a postdoctoral fellow in the research group of Prof. Tzahor
Prof. Tzahor points out that clinical trials of patients receiving the NRG1 treatment might not be overly successful if ERBB2 levels are not boosted as well. He and his team plan to continue researching this signaling pathway to suggest ways of improving the process, which may, in the future, point to ways of renewing heart cells. Because this pathway is also involved in cancer, well-grounded studies will be needed to understand exactly how to direct the cardiomyocyte renewal signal at the right place, the right time and in the right amount. “Much more research will be required to see if this principle could be applied to the human heart, but our findings are proof that it may be possible,” he noted.