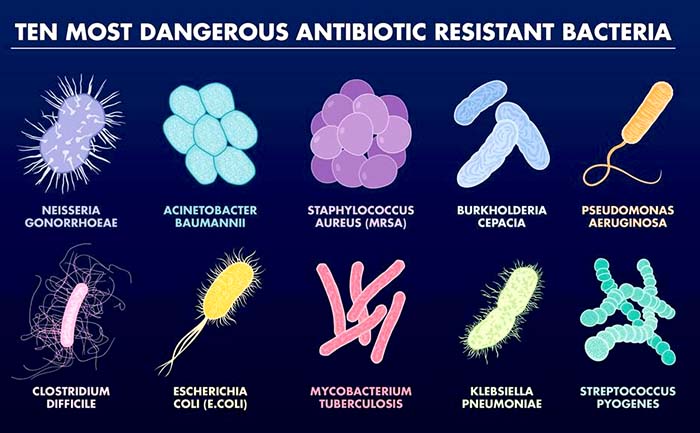
![Examples of various drug-resistant bacterial strains.[WHO]](https://genengnews.com/wp-content/uploads/2018/08/12335112811521-1.jpg)
Examples of various drug-resistant bacterial strains.[WHO]
Rapid identification of clinical samples for dangerous and drug-resistant types of bacterial infections is essential for physicians to accurately diagnose patients and administer the appropriate drug therapy. Now, new research from a team of scientists—presented recently at the 27th European Congress of Clinical Microbiology and Infectious Diseases (ECCMID)—describes a method for quickly assessing microbial pathogenesis using equipment already owned by most hospitals. The researchers presented their data in a talk entitled “Multicentre Evaluation of the BYG Carba Test v2.0, a Simplified Electrochemical Assay for the Rapid Laboratory Detection of Carbapenemase-Producing Enterobacteriaceae.”
Bacteria have been gradually evolving to become resistant to the antibiotics used to treat them. Alarmingly, over the past several years, scientists have found evidence that some bacteria have become resistant to the last-resort antibiotic called colistin. In this new study, researchers described how they were able to test bacteria to quickly tell whether they were resistant to colistin, and how easily they might pass this resistance on to other bacteria. The investigators noted that this is an important discovery because knowing which patients have these most dangerous infections means it is possible to use quarantine measures to halt their spread and stop the rise of drug resistance.
“This plasmid-encoded resistance is particularly worrying because it has the potential to spread quickly and easily and, if that happens, last-resort drugs like colistin could also become obsolete,” remarked study investigator Laurent Dortet, Ph.D., associate professor at South Paris University, France, and a researcher at Imperial College London, UK. “If, on the other hand, we can rapidly identify bacteria that have this type of resistance, we can take measures to stop its spread. This might include isolating the patient in a separate room where they are treated by dedicated medical staff.”
The research team focused their attention on the bacteria Escherichia coli and Klebsiella pneumoniae. These microbes are both members of a group of bacteria called Enterobacteriaceae that can cause gastroenteritis, urinary tract infections, lung diseases such bronchitis, and pneumonia, and even sepsis. Moreover, some strains of these bacteria have become resistant to nearly all available antibiotics, mostly by producing antibiotic-inactivating enzymes, for example, extended-spectrum lactamases and carbapenemases. This means that colistin often remains the only treatment option for these multidrug-resistant bacteria.
Previous research showed that two different types of colistin resistance exist in bacteria. One type, called chromosome-encoded resistance, can only be passed on when bacteria grow and divide to form new bacteria cells. The other type, called plasmid-encoded resistance, is considered more dangerous because it can be passed on from one type of bacteria to another completely different type of bacteria.
In the current study, the researchers tested 134 different colonies of bacteria using a mass spectrometer. Mass spectrometers are found in testing labs at most hospitals where they are used to analyze various molecules.
“The exciting thing about this technique is that it relies on technology that is already available in most hospitals,” concluded Gerald Larrouy-Maumus, Ph.D., lecturer in molecular microbiology at Imperial College London. “This means that it could be rolled out quickly and cheaply, and potentially have a rapid impact on tackling drug resistance.”