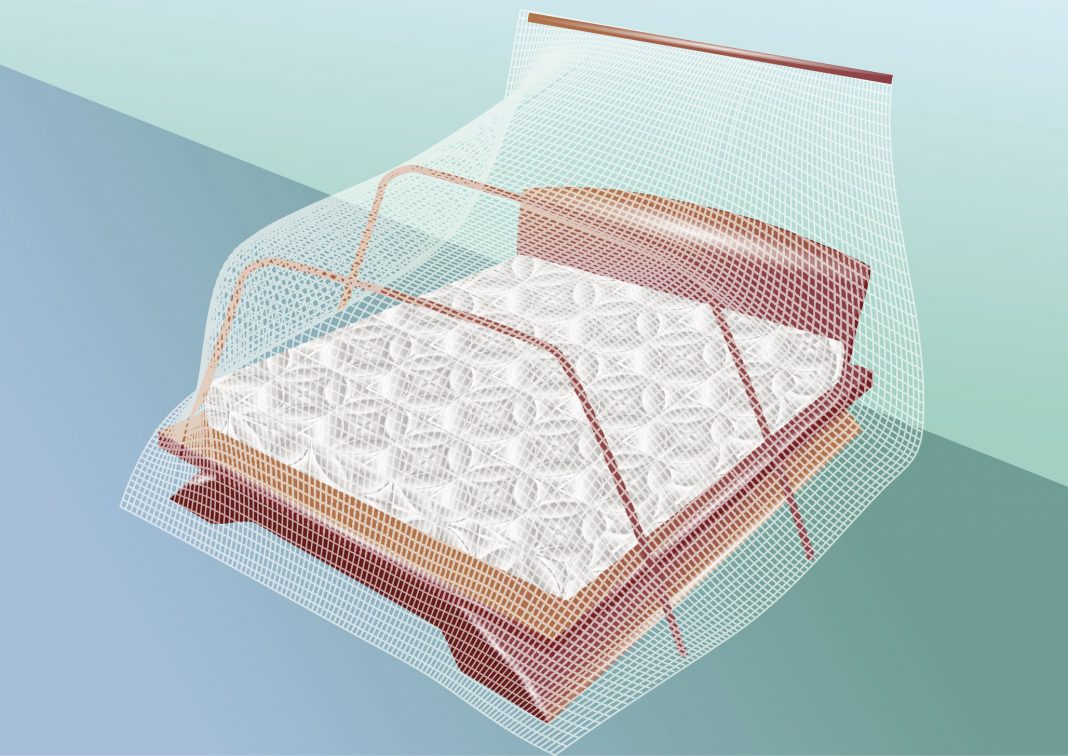
While a physical barrier may not be the best option to throw up between bordering nations, physical protection such as clothing and screens can be very effective to prevent bites from annoying pests. For instance, when used properly, insecticide-treated bed nets can reduce the transmission of malaria up to 20% and are often used in combination with various medicines to prevent and treat infections. Yet, instead of impregnating nets with a chemical that kill mosquitos, what if they were treated with an antimalarial agent that targets the parasite within the mosquitoes? Well, a team of investigators at Harvard University’s T.H. Chan School of Public Health and Virginia Tech College of Science set out to determine if this approach could be a viable option for global health officials to exploit in slowing or even preventing malaria infections.
The widespread use of the current one-two combination punch consisting of bed nets and antimalarial drugs has been very effective at reducing disease transmission rates. However, since close to 50% of the world’s population live in malaria-endemic areas there were still an estimated 219 million cases of the disease in 2017 and 435,000 deaths. With drug resistance and global temperatures on the rise, the increased threat from malaria is ever looming.
In the current study, the researchers found that using a common antimalarial drug—atovaquone—to coat mosquito bed nets “cured” the insects of the parasite, ultimately preventing it from spreading the disease. Findings from the study were published recently in Nature through an article titled “Exposing Anopheles mosquitoes to antimalarials blocks Plasmodium parasite transmission.”
In addition to covering bed nets in atovaquone, the researchers also developed computer models that explored how adding the compound to the bed nets and its ability to cure individual mosquitoes affected malaria prevalence in the human population as a whole. Childs’ modeling factored in various external conditions, such as the current malaria prevalence, bed net coverage, and level of insecticide resistance.
“We showed that the development of P. falciparum can be rapidly and completely blocked when female Anopheles gambiae mosquitoes take up low concentrations of specific antimalarials from treated surfaces—conditions that simulate contact with a bed net,” the authors wrote. “Mosquito exposure to atovaquone before, or shortly after, P. falciparum infection causes full parasite arrest in the midgut and prevents transmission of infection. Similar transmission-blocking effects are achieved using other cytochrome b inhibitors, which demonstrates that parasite mitochondrial function is a suitable target for killing parasites. Incorporating these effects into a model of malaria transmission dynamics predicts that impregnating mosquito nets with Plasmodium inhibitors would substantially mitigate the global health effects of insecticide resistance.”
The research team found that mosquitoes that sat on the surfaces for six minutes—a typical resting time on bed nets—would absorb the medicine needed to kill the malaria parasite in them. The method could be more effective and less harmful to the people and environment in malaria hotspots. It has several advantages over the current techniques.
“The mosquito should not develop resistance to the compounds because we’re just killing the parasite that’s inside it,” noted study investigator Lauren Childs, PhD, an assistant professor of mathematics in the Virginia Tech College of Science. “And atovaquone is already a licensed drug, so we know it’s safe for humans.”
Developing, getting approval for, and distributing new insecticides to which mosquitoes have not built a resistance could take too long, as malaria illnesses and deaths spread. Childs credited her colleagues at Harvard’s Chan School and the transdisciplinary team that melded her mathematical modeling skills with expertise in epidemiology, biology, public health, and other fields to offer a potential solution to a major global problem.
And it’s a solution that could possibly be implemented in time to make a difference, she said.
“The population in sub-Saharan Africa is accustomed to bed nets and already uses them,” Childs concluded. “There are a lot of reasons this could move quickly to action.”