Johnson & Johnson’s (J&J) Janssen Biotech has ended a nearly four-year-old collaboration with Geron, which as a result is regaining rights to the blood cancer candidate imetelstat, the companies said today—but is seeing its stock lose two-thirds of its value this morning.
Janssen said in a terse statement that its decision “is the result of a strategic portfolio evaluation and prioritization of assets” within its portfolio.
The companies inked an up-to-$935 million collaboration in November 2014, under which Geron gave Janssen exclusive worldwide rights to develop and commercialize imetelstat for all human therapeutic uses, including the drug’s indication of hematologic myeloid malignancies. The following year, J&J included imetelstat among a dozen candidates it projected would reach blockbuster status by 2019 by generating annual revenue of more than $1 billion.
But today, the end of the collaboration touched off a stock sell-off that sent Geron shares plummeting 71% in premarket trading this morning, to $1.81, from yesterday’s closing price of $6.23.
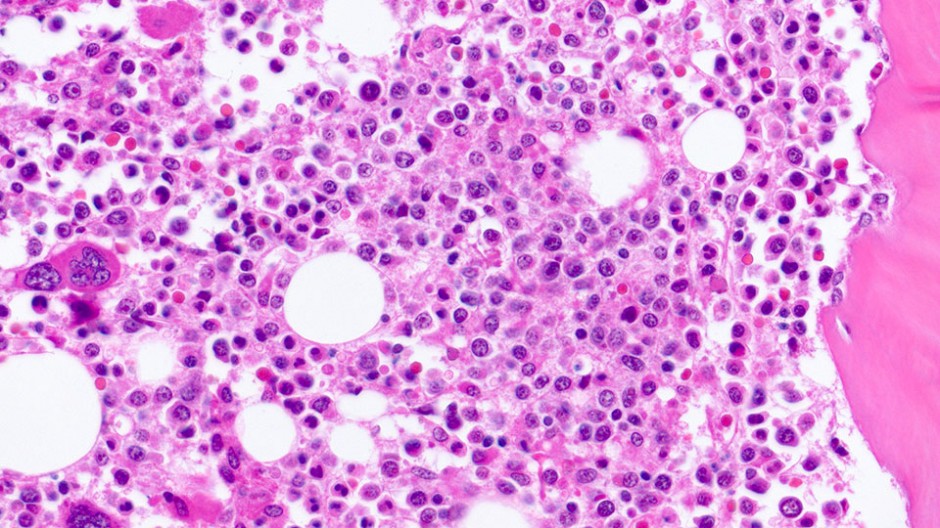
Imetelstat is a first-in-class telomerase inhibitor that has been under study in two mid-phase trials—the Phase II portion of the Phase II/III IMerge study in patients with lower risk myelodysplastic syndromes (MDS) (NCT02598661), and the Phase II IMbark trial in patients with intermediate-2 or high-risk myelofibrosis (MF) (NCT02426086).
In a separate statement, Geron disclosed results from both trials, and said it would prioritize the advancement of IMerge into Phase III next year based on data from the trial’s Phase II portion from 38 patients in initial and expansion cohorts.
IMerge’s primary efficacy endpoint is the red blood cell transfusion independence (RBC-TI) rate, lasting at least eight weeks. Key secondary endpoints include the RBC-TI rate lasting at least 24 weeks, amount and relative change in red blood cell transfusions and hematologic improvement.
In June, Geron reported IMerge Phase II results for its initial cohort of 13 patients who had not received prior treatment with either a hypomethylating agent (HMA) or lenalidomide and did not have a del(5q) chromosomal abnormality. That initial cohort showed increased durability and RBC-TI rate compared to the overall trial population (54% vs. 34%).
Expansion of Enrollment
Based on that data, the Phase II trial enrollment was expanded to include an additional 25 patients who are non-del(5q) and naïve to HMA and lenalidomide treatment, Geron said, “in order to increase the clinical experience and confirm the benefit-risk profile of imetelstat dosed at 7.5 mg/kg every four weeks in this target patient population.”
Janssen conducted an early data review of the expansion cohort or “data snapshot” since the median follow-up was less than half the time the 13-patient initial cohort had been followed when their data were first reported. In that data snapshot, Geron disclosed, the ≥8-week RBC-TI rate was 28%. In the combined 38-patient population, the ≥8-week RBC-TI rate was 37%. As of the data snapshot, sufficient time had not elapsed in the expansion cohort to assess the ≥24-week RBC-TI rate.
“Geron believes the combined data from the initial and expansion cohorts for the target patient population (n=38) support initiating the Phase III portion of IMerge to address an unmet medical need for patients who have failed ESAs [erythropoiesis stimulating agents] and for whom currently available therapies show only modest efficacy,” the company stated.
Final data from Phase II of IMerge is expected to be submitted for presentation at a future medical conference, next year, Geron said.
The planned Phase III portion of IMerge, Geron said, will be a double-blind, randomized, placebo-controlled trial in approximately 170 patients—and will begin after sponsorship of the imetelstat clinical program is transferred from Janssen.
Geron said it anticipates patient enrollment for Phase III of IMerge to begin by mid-2019. The company has retained a global CRO to support imetelstat clinical development.
No Complete Remission
For the IMbark trial, Geron disclosed primary analysis highlights showing that in the 59-patient 9.4 mg/kg dosing arm, the spleen response rate was 10% and the symptom response rate, 32%. No patients achieved complete remission, and one patient achieved partial remission.
IMbark was designed to evaluate two starting dose levels of imetelstat (either 4.7 mg/kg or 9.4 mg/kg administered by intravenous infusion every three weeks) in approximately 200 patients with Intermediate-2 or High-risk MF who have relapsed after or are refractory to prior treatment with a JAK inhibitor.
The co-primary efficacy endpoints for IMbark were spleen response rate, defined as the proportion of patients who achieve a ≥35% reduction in spleen volume assessed by imaging; and symptom response rate, defined as the proportion of patients who achieve a ≥50% reduction in Total Symptom Score, at 24 weeks. Key secondary endpoints were safety and overall survival.
At the time of the primary analysis, median overall survival had not been reached after 23 months of median follow-up. The extension phase of IMbark is ongoing to allow long-term treatment and follow-up of patients, Geron said, with data collection to consist of serious adverse events and survival.
For both IMbark and IMerge, Geron said, Janssen has submitted results for potential presentation at the 60th Annual Meeting of the American Society of Hematology (ASH), to be held December 1-4 in San Diego. If Janssen’s abstract is accepted, Geron added, it expects more mature data from both trials to be presented.