Huntington’s disease (HD) was the first neurological disorder to be linked to a mutation in a single gene—a discovery made more than 25 years ago. However, neither the pathogenic mechanisms leading to neurodegeneration nor the normal functions of huntingtin (HTT) are well understood. In addition, no therapy exists to treat or slow the progression of the disease—a fatal condition involving the death of brain cells.
HD typically strikes people in midlife. But new findings suggest the disease process starts decades earlier. Although symptoms emerge in adulthood, researchers have been able to detect the earliest effects of Huntington’s in the first two weeks of human embryonic development.
This work is published in Development, in the paper, “Huntingtin CAG expansion impairs germ layer patterning in synthetic human 2D gastruloids through polarity defects.”
The findings recast Huntington’s, often considered a neurodegenerative condition, as a developmental disease, and point to new approaches for finding treatments.
“When the patient goes to the doctor, that’s when the last dominoes have fallen. But the first domino is pushed in the developmental phase,” said Ali Brivanlou, PhD, head of the Laboratory of Synthetic Embryology at Rockefeller University. “Knowing this trajectory, we may be able to block the progression of the disease.”
Previously, researchers in the Brivanlou lab found evidence that abnormalities due to Huntingtin mutation arise decades before the neurons start to perish: In the first stages of the brain development in the embryo, when uniform cells are becoming specific brain cell types and forming structures. Introducing the Huntington’s mutation in these developing cells led to abnormal neurons and structures.
In the new study, the researchers demonstrate a “specific and highly reproducible CAG length-dependent phenotypic signature in a synthetic model for human gastrulation derived from human embryonic stem cells (hESCs).” Specifically, they wrote that they observed “reduction in the extension of the ectodermal compartment that is associated with enhanced activin signaling.”
The researchers examined the effects of Huntington’s mutation at the earlier stage of gastrulation, during which the two-week-old embryo starts to form the three embryonic germ layers, from which the progenitors of all cell types, including brain cells emerge.
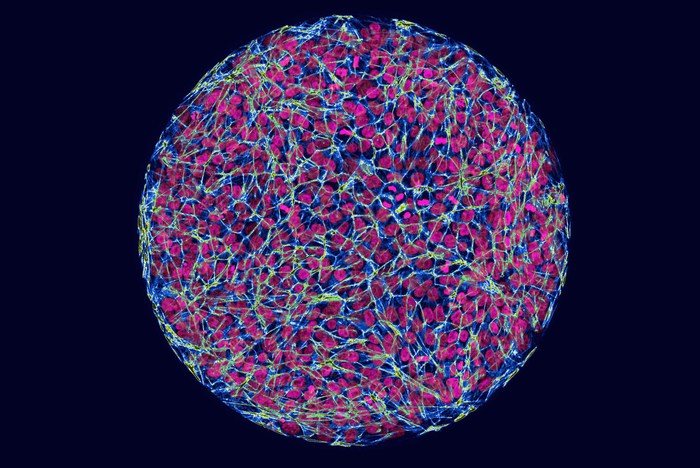
The researchers created synthetic human embryos—lab-generated embryos that are derived from stem cells and mimic the behavior of human cells during the early stages of development. They then used CRISPR/Cas9 to insert the range of Huntington’s mutations found in people with the disease into the embryos.
Comparing the embryos with and without the mutation revealed a pattern: the mutations affected the size of germ layers. And the more severe mutations led to larger differences. “It’s a phenotypic signature—you can see it with your eyes,” said Brivanlou.
That visible change, the researchers found, is caused by an alteration to a signaling pathway that guides the embryonic cells. How exactly such early changes affect the development of embryos later on is unclear. But people with these mutations are born and function normally for years. Researchers suspect that a developing embryo uses certain mechanisms to compensate for the deleterious effects of Huntington’s mutations. “Understanding those mechanisms may be the key to developing new treatments that delay the symptoms, or even cure the disease,” Brivanlou said.
Using synthetic human embryos as their platform, the researchers have started to screen for drugs that can correct these abnormalities. This approach, they hope, will lead to developing clinical interventions that will address the causes of Huntington’s disease, and not just the consequences.