Out-of-place DNA arouses the suspicion of a mammalian protein called cGAS, or cyclic GMP-AMP synthase. Although cGAS is usually as passive as a bored security guard, it leaps into action when it comes across DNA in the cell’s cytosol. Such DNA may indicate a foreign or cancerous intrusion.
Curiously, the human version of cGAS has unique structural features that keep it on the lookout for long sequences. Short sequences often get a pass.
The advantages of a bias against long pieces of stray DNA aren’t exactly clear. Perhaps the bias helps prevent autoimmune disorders. In any case, the structural details behind the bias could inform the development of immunotherapeutic drugs, including drugs to combat cancer.
Contributing to a deeper understanding of these issues is a recent study conducted by scientists at Harvard Medical School and the Dana-Farber Cancer Institute. These scientists have, for the first time, identified the structural and functional differences in human cGAS that set it apart from cGAS in other mammals and underlie its unique function in people.
The human-specific cGAS structural and functional features were described July 12 in the journal Cell, in an article titled, “Structure of the Human cGAS–DNA Complex Reveals Enhanced Control of Immune Surveillance.” This article describes how the scientists used reconstitution of cGAMP signaling in bacteria to determine that human cGAS regulation could be attributed to two amino acid substitutions in the DNA-binding surface.
“Human-specific substitutions are necessary and sufficient to direct preferential detection of long DNA,” the article’s authors wrote. “Crystal structures reveal why removal of human substitutions relaxes DNA-length specificity and explain how human-specific DNA interactions favor cGAS oligomerization.”
These findings may inform the design of small-molecule drugs tailored to the unique structural features of the human protein—an advance that promises to boost the precision cGAS-modulating drugs that are currently in development as cancer therapies.
“Several promising experimental immune therapies currently in development are derived from the structure of mouse cGAS, which harbors key structural differences with human cGAS,” said the study’s senior author, Philip J. Kranzusch, Ph.D., assistant professor, microbiology and immunobiology, Harvard Medical School. “Our discovery should help refine these experimental therapies and spark the design of new ones. It will pave the way toward structure-guided design of drugs that modulate the activity of this fundamental protein.”
When cGAS detects out-of-place DNA, it makes another chemical—a second messenger—called cGAMP, thus setting in motion a molecular chain reaction that alerts the cell to the abnormal presence of DNA. At the end of this signaling reaction, the cell either gets repaired or, if damaged beyond repair, it self-destructs. But the health and integrity of the cell are predicated on cGAS' ability to distinguish harmless DNA from foreign DNA or self-DNA released during cell damage and stress.
The current study reveals the evolutionary changes to the protein's structure that allow human cGAS to ignore some DNA encounters while responding to others.
For their work, the team turned to an unlikely collaborator–Vibrio cholerae, the bacterium that causes cholera, one of humankind's oldest scourges.
Taking advantage of a cholera enzyme that shares similarities with cGAS, the scientists were able to recreate the function of both human and mouse cGAS in the bacterium.
In a series of experiments, the scientists observed activation patterns between the different types of cGAS, progressively narrowing down the key differences that accounted for differential DNA activation among the three.
The experiments revealed that out of the 116 amino acids that differ in human and mouse cGAS, only two accounted for the altered function of human cGAS. Indeed, human cGAS was capable of recognizing long DNA with great precision but it ignored short DNA fragments. The mouse version of the protein, by contrast, did not differentiate between long and short DNA fragments.
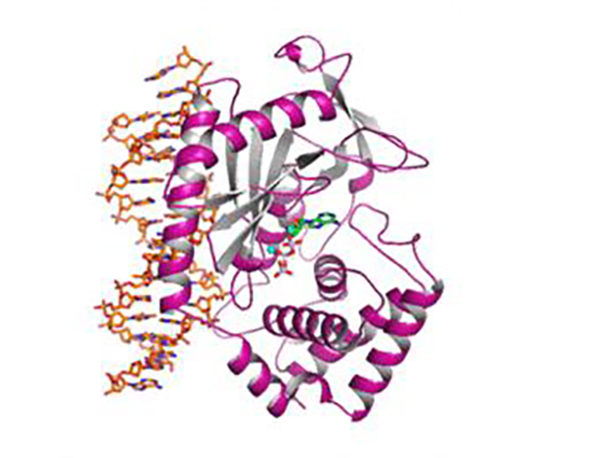
In a final set of experiments, the team determined the atomic structure of the human cGAS in its active form as it binds to DNA. To do so, the team used a visualization technique known as X-ray crystallography, which reveals the molecular architecture of protein crystals based on a pattern of scattered X-ray beams.
Profiling the structure of cGAS “in action” revealed the precise molecular variations that allowed it to selectively bind to long DNA, while ignoring short DNA.
“Understanding what makes the structure and function of human cGAS different from those in other species was the missing piece,” Dr. Kranzusch says. “Now that we have it, we can really start designing drugs that work in humans, rather than mice.”