New research suggests that the presence of certain bacteria in a gut biome may be an indicator of colon polyps that will become cancerous. Researchers from the University of Washington School of Medicine analyzed 40 patients who had undergone colonoscopies and had biopsies taken near polyps to identify bacteria and compare with those who were polyp-free.
Their findings are published in the journal Cell Host & Microbe in a paper titled, “Genomic and functional characterization of a mucosal symbiont involved in early-stage colorectal cancer.”
“Colorectal cancer (CRC) is a major health concern worldwide,” the researchers wrote. “Growing evidence for the role of the gut microbiota in the initiation of CRC has sparked interest in approaches that target these microorganisms. However, little is known about the composition and role of the microbiota associated with precancerous polyps. Here, we found distinct microbial signatures between patients with and without polyps and between polyp subtypes using sequencing and culturing techniques.”
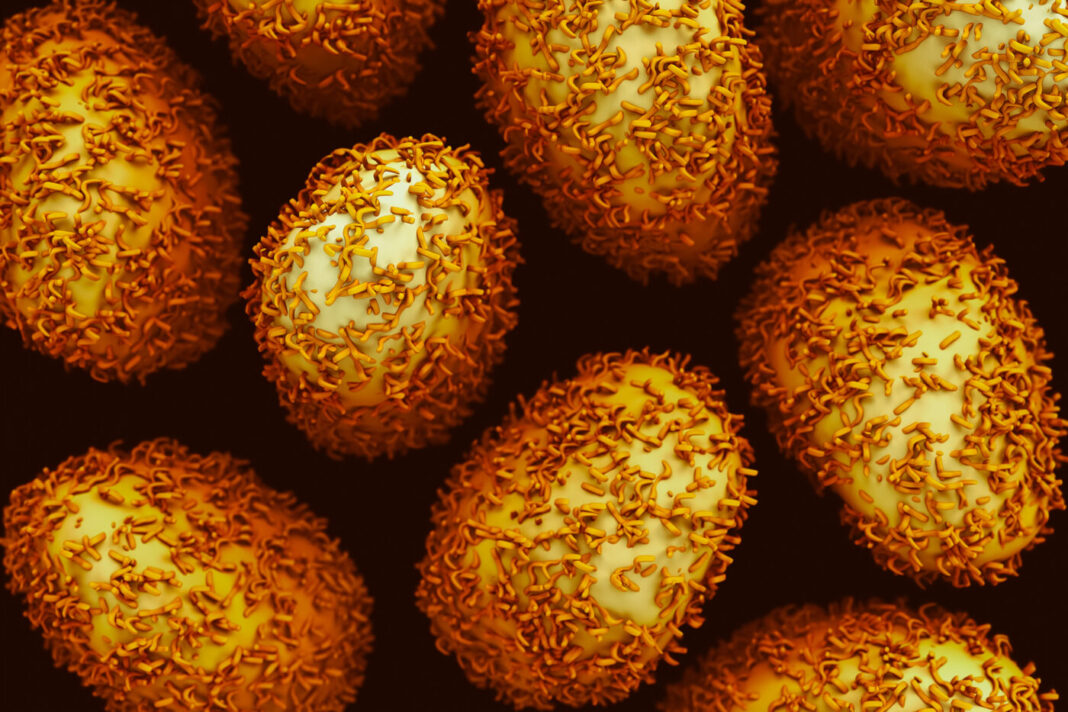
The research was led by William DePaolo, PhD, associate professor at the University of Washington School of Medicine. He and his team discovered that the bacteria Bacteroides fragilis, was elevated in the mucosal biopsies of patients with polyps.
“The whole idea is that most people look at advanced colorectal cancer and think of the microbiome, but it’s hard to determine if the microbiome has changed and when it changed,” DePaolo explained. “So we took an earlier look at the disease and asked when might the microbiome may be pushing a polyp toward cancer.”
Also, when people think of the microbiome and its role in disease, they often think of compositional changes where a potentially dangerous bacteria takes over, he added.
“What our data suggests is that, in order to survive within an environment where metabolic and inflammatory changes are occurring, a normally healthy gut and related bacteria may adapt in such a way that causes it to contribute to the inflammation rather than suppress it,” DePaolo explained.
The next step, he said, is to expand the study to 200 patients to determine whether a fecal sample might be used as a surrogate for the mucosal biopsy.