Blocking the cytokine tumor necrosis factor (TNF), which drives chronic inflammation and cell death in the intestine, provides therapeutic benefit to patients with inflammatory bowel disease (IBD). However, the pathways that protect the intestine from TNF are incompletely understood.
Now, a team of researchers has shown that heparin-binding epidermal growth factor–like growth factor (HB-EGF) is produced in response to gut inflammation by a set of immune-regulating cells called ILC3s. These immune cells reside in many organs including the intestines, though their numbers are known to be depleted in the inflamed intestines of IBD patients.
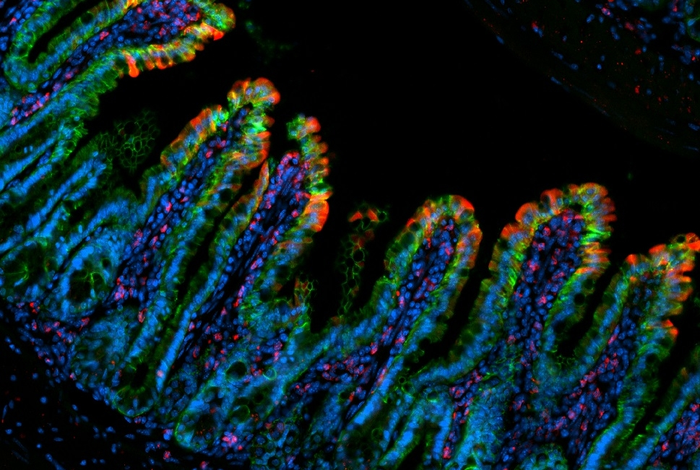
The researchers showed in mouse experiments that HB-EGF can powerfully counter the harmful effects of TNF. In doing so, ILC3s protect gut-lining cells when they would otherwise die and cause a breach in the intestinal barrier.
This work is published in Nature Immunology, in the paper, “Group 3 innate lymphoid cells produce the growth factor HB-EGF to protect the intestine from TNF-mediated inflammation.”
“We’ve discovered a new cellular pathway that is essential to protect against gut inflammation. This discovery could lead to a better understanding of IBD pathogenesis and new strategies to treat this disease” said Gregory Sonnenberg, PhD, associate professor of microbiology and immunology in medicine at Weill Cornell Medicine.
IBD, a disease category including ulcerative colitis and Crohn’s disease, features chronic gut inflammation and many potential follow-on effects including arthritis and colorectal cancer.
Sonnenberg and colleagues recreated an IBD-like condition in mice using high doses of TNF. They found in these experiments that ILC3s strongly protect the gut linings of the mice from TNF-induced inflammatory damage—mice lacking ILC3s suffered significantly worse damage.
Prior studies have suggested that ILC3s help protect the gut at least in part by producing IL-22, which promotes gut barrier function. However, the mouse experiments in the new study indicated that ILC3s’ gut-protecting effect against TNF works independently of IL-22.
Single-cell RNA sequencing allowed the researchers to zero in on the mechanism of ILC3s’ protective effect: the growth factor protein HB-EGF, which they showed could specifically keep gut-lining cells alive in the presence of excessive TNF.
The team found that ILC3s are the dominant producers of HB-EGF in the gut. They were able to identify the cascade of signaling factors that occurs downstream of TNF and causes ILC3 to switch on HB-EGF production—and they observed the same cascade in human ILC3s, indicating that these findings are not just specific to mice. The researchers also confirmed from analyses of IBD-patient gut tissue that HB-EGF-producing ILC3s are reduced in areas of gut inflammation.
The findings reveal a key mechanism that the gut normally uses to protect itself from harmful inflammation and suggest that the loss of ILC3s is at least one reason this mechanism fails in IBD.
“Identifying the significance of this pathway is a good first step, and we’re now thinking about how we might manipulate this pathway to benefit IBD patients,” Sonnenberg said.
The loss of ILC3s in the IBD gut poses a challenge to the development of therapeutic solutions that depend on ILC3s, he noted. Moreover, though HB-EGF on its own could be therapeutic, even if ILC3s are depleted, HB-EGF has been linked to the faster growth of a variety of cancers.
“Our ongoing research is interrogating the role of this ILC3 and HB-EGF pathway in the development of chronic-inflammation-related colon cancer,” said Lei Zhou, PhD, postdoctoral associate in the Sonnenberg laboratory. “It will be important to delineate the exact cellular and molecular mechanisms by which this novel pathway coordinates intestinal health, inflammation, and cancer before moving forward with manipulating it as a therapeutic strategy.”