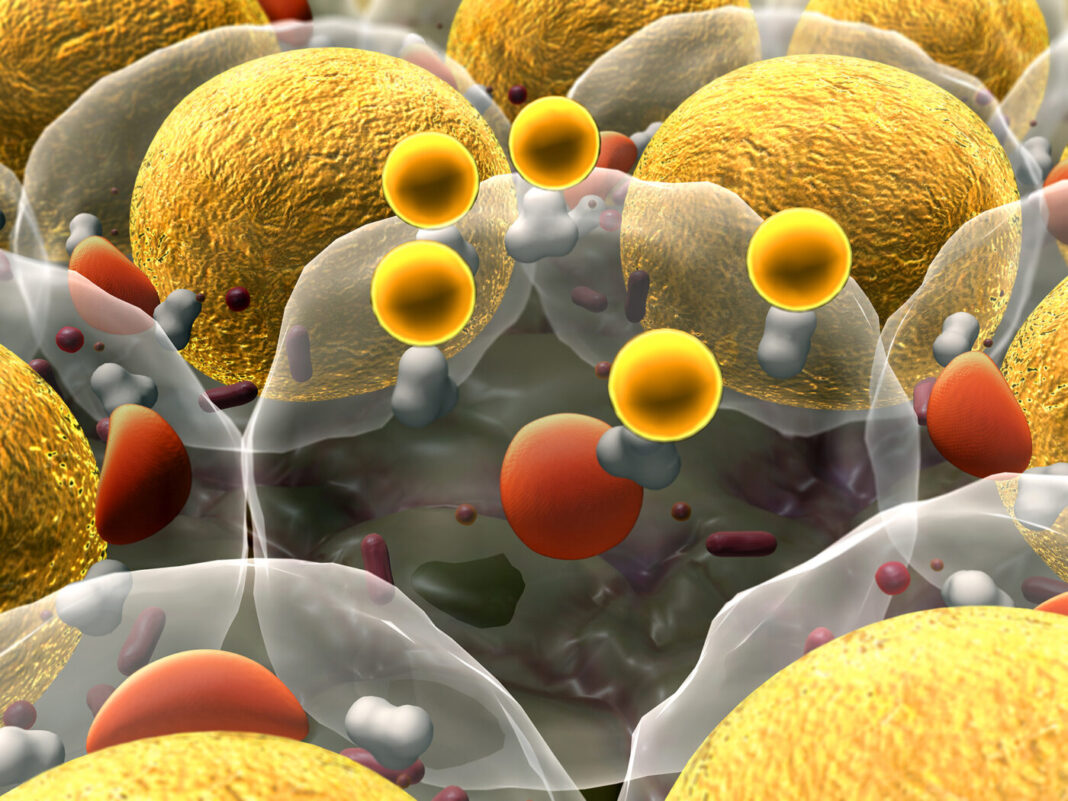
Researchers in the U.K. have discovered that human fat cells have their own internal clocks and circadian rhythms that impact on key metabolic functions and core aspects of cellular biochemistry. The scientists, headed by Jonathan Johnston, reader in chronobiology and integrative physiology at the University of Surrey, say the results from their studies in human volunteers provide new insights that could have clinical implications. “The circadian timing system thus has an intimate relationship with many core aspects of human physiology and pathways relevant to therapeutics,” they wrote in their published paper in Scientific Reports, which is titled, “Circadian regulation in human white adipose tissue revealed by transcriptome and metabolic network analysis.”
Many aspects of human metabolism show daily variations, and these are due, in part, to the body’s inbuilt circadian timing system, the researchers explained. This internal rhythm system comprises a central “master” clock in the hypothalamus within the brain, and an integrated network of circadian clocks that are present in all the body’s major tissues. Circadian disruption is a cause of abnormal metabolic physiology, and has been linked with obesity and other detrimental physiological aspects of working night shifts. “Misalignment of human clocks with each other and the environment is believed to be a major contributor to obesity and related pathologies associated with shift work,” the team wrote.
It’s estimated that nearly half of all mouse genes exhibit a circadian expression profile in at least one tissue, and many of these genes are integral to physiological function. However, carrying out similar transcriptomic studies to study rhythmic gene expression in people isn’t easy because we can’t take samples from every human tissues, other than blood.
For their latest studies focused on investigating circadian rhythms in the expression of genes in human fat, or white adipose tissue (WAT), the University of Surrey team recruited 7 human volunteers. The participants, who were all male, underwent regulated sleep-wake cycles and meal times outside the laboratory, and then came into the laboratory, where they maintained the same sleep-wake and mealtime routine. The participants then experienced a 37-hour “constant routine,” during which there were no changes in light-dark, feed-fast, and sleep-wake cycles. “Unmasking of circadian rhythms in a constant routine protocol permits removal/minimization of rhythmic changes in the environment, feeding behavior, and sleep-wake physiology, which are known to influence 24-hour rhythm,” the team noted.
They took biopsies of fat tissue from each participant every six hours, to carry out transcriptomic analysis. The results identified 727 genes in fat tissue that expressed their own circadian rhythm, independent of external influences such as light or feeding. About a third of the genes showed peak expression in the morning, and the other two-thirds peaked in the evenings. Many of the genes were involved in key metabolic functions. Morning-peaking transcripts included those of genes associated with regulating gene expression and nucleic acid, while gene transcripts peaking in the evening were associated with redox activity and organic acid metabolism. As might be expected, “the most common rhythmic processes in human subcutaneous white adipose are those linked to fatty acid metabolism,” the authors wrote. Interestingly, a comparison of the gene transcript results from human fat with those of previous rhythmic transcript studies in human blood, and in animal fat, suggested that there was only a partial overlap of circadian genes. Thirty-two transcripts exhibiting circadian rhythmicity in mouse white adipose tissue were also classified as rhythmic in the team’s human fat study, while only 14 genes were rhythmic in both the human and independent baboon white adipose tissue datasets. A comparison of human adipose data and previous human blood data found 14 common rhythmic genes.
“Circadian genes that were common to human adipose tissue and at least one of the blood datasets were involved in fundamental processes for cell function; namely circadian rhythm regulation, metabolic processes, and transcription and translation,” the authors wrote. “The low overlap between circadian transcriptomes in human and mouse adipose tissue could derive from species differences as well as different physiological properties of the adipose depots.”
The team also looked at the functional consequences of the transcriptomic data, by looking at molecular interactions and metabolic pathways. The results supported the suggestion that adipose circadian rhythms play key roles in fatty acid metabolism, nucleic acid metabolism, and other key aspects of cell function such as the citric acid cycle. “In silico pathway analysis further indicated circadian regulation of lipid and nucleic acid metabolism; it also predicted circadian variation,” they stated. “These novel findings indicate the association of circadian processes with specific and critical metabolic pathways in cellular metabolism of human white adipose tissue.”
“Tissues made up of fat cells don’t just store excess energy, they are active metabolic tissues, full of their own rhythms,” Johnston said. “This is the first time that we have been able to identify such rhythms in human fat. This provides us with more information about how human metabolism changes across the day and possibly why the body processes foods differently during day and night.”